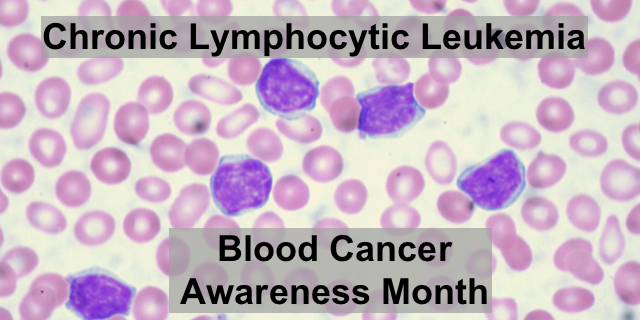
CLL or Chronic Lymphocytic Leukemia results from a mutation in B lymphocytes, a type of white blood cell that develops in the bone marrow. B-cells produce antibodies, an important part of the immune system. CLL can be slow growing, with small slow changes in the blood counts over years or fast growing, where cancerous B-lymphocytes crowd out the bone marrow, making it difficult for other blood cells, like platelets and red blood cells, to be produced.
In 2008, Dr. Brian Koffman, a family practice physician started a blog because he had made a risky decision. Koffman had had CLL for three years. His CLL had stabilized and he decided to undergo an elective bone marrow transplant. An exact-match blood donor had been found. He wrote,
Most people wait for their HSCT as a “Hail Mary” desperation last move. I am doing it from a very healthy and quite elective position. I haven’t even had any real chemo yet. I have other cards I could play, but I have the perfect donor and a deep remission and my good health so I am gambling it all.
Dr. Koffman’s gamble had mixed results. The bone marrow from his donor did not engraft. However, the pre-treatment chemotherapy used to kill off the lymphocytes in his bone marrow actually put his cancer into remission.
Although he is a physician, he describes experiences he has as a hospitalized patient like,
I have had about 25 minutes contact time with the discharge staff in the last 8 and 1/2 hours. Still at the hospital waiting for my prescriptions and PICC supplies and masks and final instructions.
A transformation began to take place in Dr. Koffman. As he faced more of the challenges of patients, he became an activist for patients.
Our voices must be heard at the meetings between researchers and funders on how trials are set-up, at IRB (institutional review boards) that approve those trial designs and any subsequent revisions, payors who decide what treatments get covered and what don’t, and of course in our doctors’ offices when we are planning our therapy using a shared decision making model.
By the end of 2008, Dr. Koffman began a yearly pilgrimage to the American Society of Hematology (ASH) Annual meeting. From these meetings he reported important clinical trials and news to followers of his blog. At the December 2011 ASH meeting he learned of a phase I, II Clinical Trial happening at Ohio State University which would take patients who had had stem cell transplant. The clinical trial tested the safety and efficacy of PCI 32765 and Ofatumumab. As before, he took the risk and began in the clinical trial which eventually led to FDA approval of ibrutinib at the end of July 2014. This medication kept him in remission until 2018. Again he reported in his blog,
I have no problem with the idea of enrolling in a trial. On the contrary, …we cherish trials as the place to get the best and latest care. I am alive today because I entered an early trial six years for the game changing small molecule, PCI-32765, now known as ibrutinib. I am deeply grateful for the time and quality of life that choice provided me….It was the best move I could have made.
And I am planning to repeat a similar process now.
Dr. Koffman enrolled in a CAR T-cell clinical trial. He is alive and well and has started a non-profit which provides educational information, curated by top hematology oncologists, specifically for patients with CLL. He is also a member of the Leukemia and Lymphoma Society. The Leukemia and Lymphoma Society has an excellent booklet with information on CLL and other blood cancers.
References:
- http://bkoffman.blogspot.com/
- https://www.lls.org/
- https://cllsociety.org/
Feature image: Ed Uthman / CC BY-SA (https://creativecommons.org/licenses/by-sa/2.0)






Bom dia
Meu nome é Daniel, residente em Araras-SP-Brasil, tenho LLC desde 2009 e após vários tratamentos que fiz, não tive boa resposta, sempre com PLAQUETOPENIA, cheguei a ter 7 mil platquetas.
Há exatamentes 17 meses comecei tomar o Ibrutinib (420 mg/dia). e as plaquetas no ultimo exame foram a 169 mil e os leucocitos há 7 mil, vivo uma vida normal e estou muito bem.
Daniel
So happy that you are doing better with ibutrinib. Thank goodness there are new treatments for CLL available! Best Kathleen