When we posted, “What’s in a name? Rheumatoid Arthritis versus Rheumatoid Disease,”we featured Kelly Young, a mom on a crusade to change thinking about an autoimmune disease that attacks the connective tissue of joints and systemically attacks the organs of the body – rheumatoid disease. Rheumatoid disease (also known as rheumatoid arthritis) affects people of all ages. It can impact life expectancy by 10 to 15 years, due to its effect on the heart and lungs and because it increases risk of infections and cancer.
As Shai Bearden, a 32-year old mother of three and rheumatoid disease patient described in The Mighty,
“When people think of rheumatoid arthritis (RA), they often think of older people with joint pain. In reality, RA is an extremely dynamic, multi-faceted illness. ..It’s an auto-immune disease…[that] causes…fatigue, pain, sight problems, headaches, nerve and muscle pain and weakness – an extensive laundry list of related issues.”
The disease progresses from small joints in the fingers or wrists on both sides of the body to inflamed, larger joints. The spleen may enlarge, impacting the number of healthy red and white blood cells and 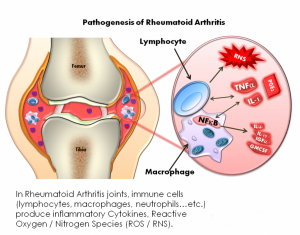 platelets, causing a higher risk of infection and bleeding. The hearts, lungs and eyes as well as the spinal cord can become inflamed. Katie Burkes wrote of her experience in 2016,
platelets, causing a higher risk of infection and bleeding. The hearts, lungs and eyes as well as the spinal cord can become inflamed. Katie Burkes wrote of her experience in 2016,
“Micro-vascular arteries in my heart [were] not working properly due to chronic high levels of inflammation from my RA…My cardiologist and my rheumatologist referred me to the Mayo Clinic cardiology team for a full work-up. I got an official diagnosis of cardiac syndrome X, also known as microvascular angina. My condition causes me to be at increased risk of a heart attack and have chronic chest pain.”
Causes of Rheumatoid Disease
Researchers have not pinned down the cause of rheumatoid disease. It is not inherited, but people who have a certain type of human leukocyte antigen (HLA) genes are more susceptible to rheumatoid disease. However, not everyone with these HLA genes will get rheumatoid disease. Triggers like smoking, stress or a viral or bacterial infection increase the likelihood of developing rheumatoid disease.
There is no cure for this condition; the goal of treatment is remission or slowing the progression of the disease.
Available Treatments for RD
There are a number of medications that are used to treat RD. Here is an explanation of what they are and what they do.
![]() Non-steroidal anti-inflammatory drugs: Like Advil or Aleve, these medications help to reduce pain and inflammation, but they do not stop damage to joint tissue.
Non-steroidal anti-inflammatory drugs: Like Advil or Aleve, these medications help to reduce pain and inflammation, but they do not stop damage to joint tissue.
![]() Disease-modifying anti-rheumatic drugs (DMARDs): These are chemotherapeutic drugs like, methotrexate (Rheumatrex, Trexall), taken at much lower doses than when they are given for cancer treatment. Others include hydroxychloroquine (Plaquenil), sulfasalazine (Azulfidine), and leflunomide (Arava). They suppress the immune system to help slow progression of RD and can stop joint tissue damage. Unfortunately, they increase the risk of infection and liver damage. They can also increase the risk of cancers like lymphoma.
Disease-modifying anti-rheumatic drugs (DMARDs): These are chemotherapeutic drugs like, methotrexate (Rheumatrex, Trexall), taken at much lower doses than when they are given for cancer treatment. Others include hydroxychloroquine (Plaquenil), sulfasalazine (Azulfidine), and leflunomide (Arava). They suppress the immune system to help slow progression of RD and can stop joint tissue damage. Unfortunately, they increase the risk of infection and liver damage. They can also increase the risk of cancers like lymphoma.
![]() Biological medications: The National Cancer Institutes (NCI) defines biologics as, “A substance that is made from a living organism or its products and is used in the prevention, diagnosis, or treatment of cancer and other diseases. Biological drugs include antibodies, interleukins, and vaccines. Also called biologic agent and biological agent.”
Biological medications: The National Cancer Institutes (NCI) defines biologics as, “A substance that is made from a living organism or its products and is used in the prevention, diagnosis, or treatment of cancer and other diseases. Biological drugs include antibodies, interleukins, and vaccines. Also called biologic agent and biological agent.”
TNF inhibitors
For RD, biologics target the factors that drive inflammation. One protein that causes inflammation is tumor-necrosis factor (TNF). There are several biologics that inhibit TNF: certolizumab (Cimzia), etanercept; (Embrel), Golimumab (Simponi), adalimumab (Humira), infliximab (Remicade).
is tumor-necrosis factor (TNF). There are several biologics that inhibit TNF: certolizumab (Cimzia), etanercept; (Embrel), Golimumab (Simponi), adalimumab (Humira), infliximab (Remicade).
TNF inhibitors increase the risk of serious infections, especially pneumonia or skin infections.
Interleukin-6 antibodies, Interleukin-1 (IL-1) Blocker
Interleukins are a kind of cytokine, a messenger molecule. Interleukin-1 and 6 are immune system proteins that stoke inflammation. Antibodies are created that block the place where interleukin-6 attaches to immune cells, thus interfering with the inflammation process. Sarilumab (Kevzara) and tocilizumab (Actemra) are two human monoclonal antibodies available to treat RD. Anakinra (Kineret) blocks the action of interleukin-1.
Interleukin-antibodies increase the risk of infection and raise liver enzymes, which may mean liver damage is occurring.
Antibodies Targeting B Cells
Rituximab (Rituxan) is a mix of mouse and human monoclonal antibodies that targets and wipes out B-cells. A risk of infection is associated with this treatment.
Targeting T-Cells
Another biologic acts on T-cells, attaching to the surface of T-cells, blocking any communication between them. Again, risk of infection is associated.
Corticosteroids: These are medications, like Prednisone, that are used to reduce swelling, inflammation and pain. They are not recommended for long term use.
Biosimilars: Biological medications are very expensive to produce and the cost is pushed onto the patient. Because of this, biosimilars are being created. Biologicals are unique types of 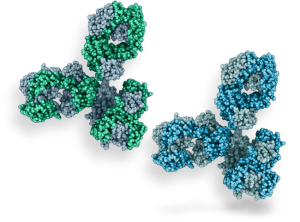 medication because they are made from living cells. Biosimilars are made with less expensive techniques and must be able to work as safely and as effectively as biological reference drugs.
medication because they are made from living cells. Biosimilars are made with less expensive techniques and must be able to work as safely and as effectively as biological reference drugs.
Staying up-to-date on treatments is made easier by signing up for Medivizor. For example, a study you would receive in your email box would tell you about a less expensive biosimilar than the one that you are using right now. In, “Is an infliximab biosimilar safe and effective for methotrexate-resistant rheumatoid arthritis?,” Medivizor describes a study of a new biosimilar that is being tested.
Living with Rheumatoid Disease
Life with RD is a roller coaster ride as Shai Bearden explained in her post on The Mighty,
“Suddenly, the world is drunkenly blurry even with my glasses on. I have weird nerve pain on my scalp that feels like fire to touch, along with dizziness and headaches, all because the inflammation in my neck is pressing on nerves at the top of my spine. My feet go numb and my legs go weak because the inflammation in my lumbar spine is pressing on those nerves, too. About a month ago, I noticed I suddenly have the beginnings of three rheumatoid nodules on my finger joints. I’ve had problems zipping my boots, turning the key in the door, and my fingers don’t want to type or hold my phone so I can text. And the hardest? I’ve almost dropped my son several times when trying to put him in his swing or picking him up.”
On the other hand, medications have transformed the life of Simone Cavanaugh, Co-founder of the non-profit, Pivot International. Her non-profit’s mission–improving the independence, mobility and quality of life of physically disabled children–comes from her life experiences as a child and adult living with RD. You can hear what she has to say below.






Are there lifestyle changes to be done by patients with RA?