In July 2015, Medivizor introduced us to a project being conducted by the Broad Institute in conjunction with Dana Farber Cancer Institute called The Metastatic Breast Cancer Project or MBC Project. In October of 2015, after two years of work involving patient input and partnership, the MBC Project website went live.
One of the reasons why this project is so important is it is patient informed and included.  According to Nikhil Wagle, MD (@Nikhilwagle), Deputy Director, Center for Cancer Precision Medicine, a collaborative between Dana Farber and Brigham and Women’s Hospitals and The Broad Institute, “The idea around the study is that we should be able to partner with patients in this research using social media and advocacy groups in order to accelerate this research.”
According to Nikhil Wagle, MD (@Nikhilwagle), Deputy Director, Center for Cancer Precision Medicine, a collaborative between Dana Farber and Brigham and Women’s Hospitals and The Broad Institute, “The idea around the study is that we should be able to partner with patients in this research using social media and advocacy groups in order to accelerate this research.”
Reaching patients with breast cancer is difficult for researchers. Eighty-five percent of all patients with breast cancer in the US are treated at community hospitals rather than large academic research centers. Only 5% of cancer patients participate in clinical trials. Patients, medical records, health information and tumor samples are dispersed all over the country.
Access to that missing data could be instrumental to finding treatment options that actually cure this terrible disease.
Since October, the MBC Project website has had over 3000 men and women with metastatic breast cancer in the US press the button, “count me in,” to in dicate an interest in being a part of the project.
dicate an interest in being a part of the project.
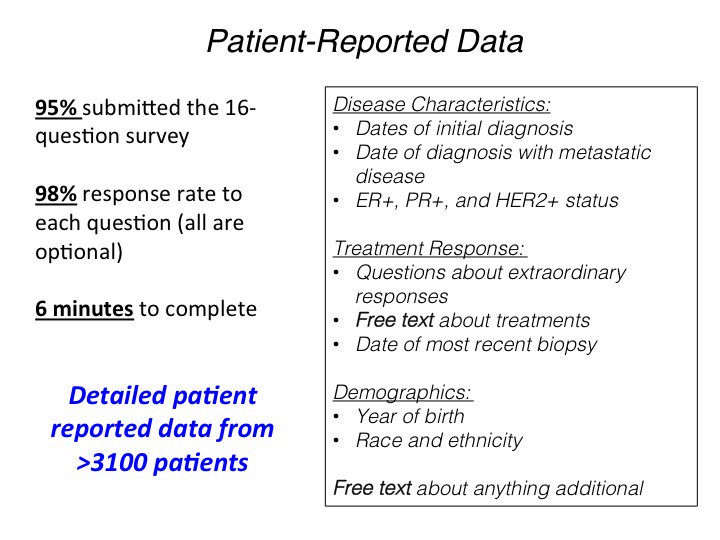
Once they click that button, there is a simple survey which asks for date of initial diagnosis, date of diagnosis with metastasis, and the type of breast cancer the person was first diagnosed with: ER (estrogen receptor status), PR (progesterone receptor status), and HER2 status. There is a question about extraordinary responses to treatment and the survey provides opportunities for people to write what they think is important for the researchers to know. Finally, they ask for the date of most recent biopsy and the year of birth, race and ethnicity. Of the over 3000 who clicked the button, 95% have answered 98% of the questions: a remarkable completion rate.
Preliminary Results
The MBC Project presented some preliminary data from the first year at the San Antonio Breast Cancer Symposium held in December 2016. Dr. Wagle presented the poster to Facebook followers.
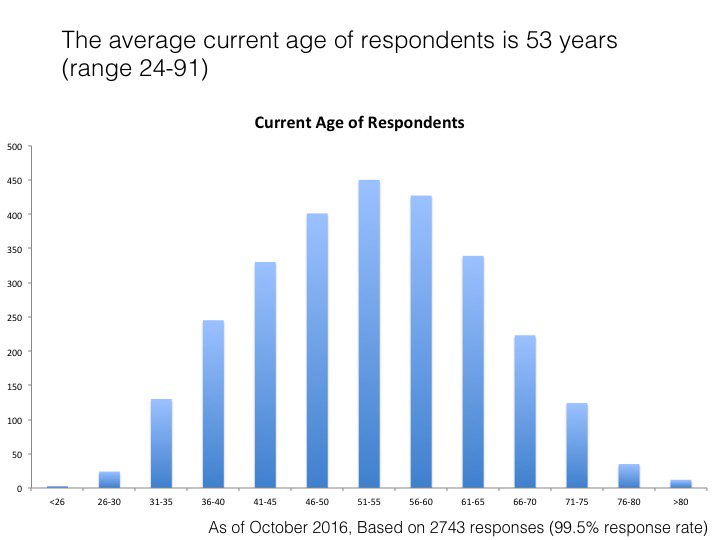
Age
The participants, so far, are young with an average current age of 53. Nine hundred and six (34%) are under the age of 40. One respondent is less than 26 years old.
Type of Breast Cancer at Diagnosis
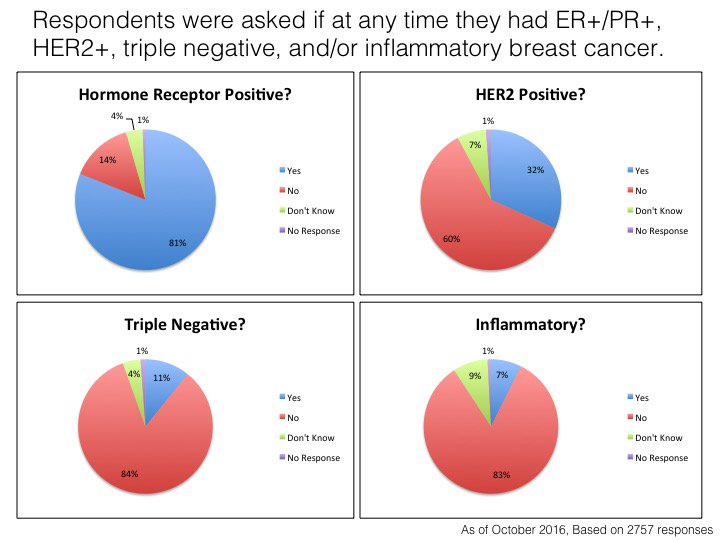
Eighty-one percent of these metastatic respondents are hormone receptor (estrogen and progesterone) positive and 32% are HER2 (human epidermal growth factor 2) positive. Only 11% are triple negative and only 7% have inflammatory breast cancer.
Self-Reported Exceptional Responses
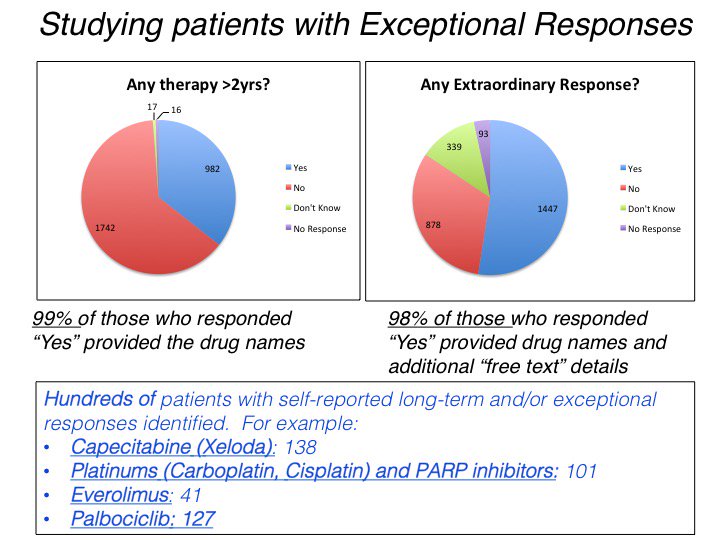
Nine hundred and eight-two patients have been on a treatment for more than 2 years. This is considered a good response to therapy. Over 1400 said that one of their treatments provided a dramatic or extraordinary response, meaning their cancer got better for a period of time.
Medications that provided these extraordinary responses included Capecitabine (xeloda), Platinums or Parp inhibitors, everolimus and palbociclib (ibrex).
A small number of participants, over 150 patients have had exceptional responses resulting in increased longevity. They have been living for more than 10 years with metastatic breast cancer.
Studying Exceptional Responders to treatments in a variety of cancers is a important new research area. This type of work looks at the genetic profile of the cancers of these Exceptional Responders to find out why they were cured. Once researchers know this, they match cancers of other people that have the same genetic profile as the cancer that is cured.
In addition, cancers of different organs can have the same genetic profile. So a drug that cures someone of thyroid cancer can potentially be used to cure someone else of ovarian cancer.
De Novo Metastatic Breast Cancer
When you are first diagnosed with breast cancer and it is metastatic at diagnosis, this is called “de novo” metastatic breast cancer. Approximately 6 % of patients with breast cancer are diagnosed with de-novo distant metastases. Yet 36% of patients in this group reported that their cancer is de novo. There are differences in risk of death and overall survival for those who have de novo metastatic breast cancer compared to those whose breast cancer relapsed.
The Numbers
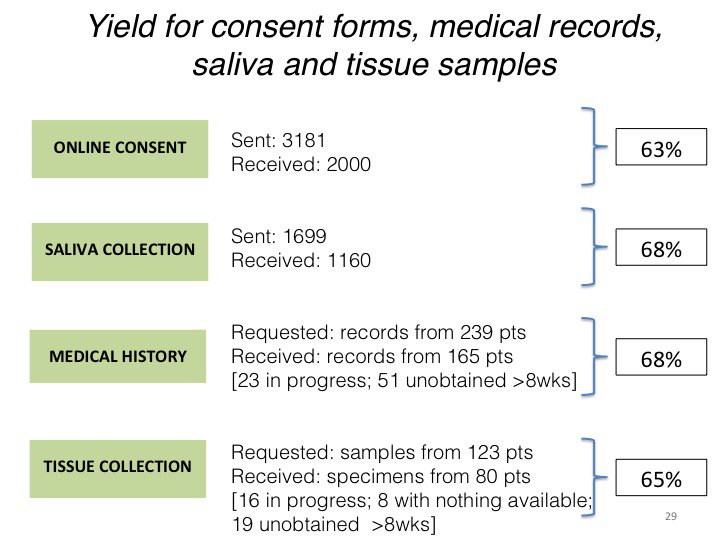
Although over 3000 people were interested in the project, there is always attrition, or a loss in numbers, as a project moves forward. For example, after filling out the preliminary form, fewer people signed the consent form. Of the people who agreed to genetic testing via saliva collection, fewer were received.
The research group requested medical records from the hospitals and physicians of 239 patients, but received 165. Of those they requested tumor samples from 123, they have only received specimens from 80 patients. Finally 90 samples from 49 patients were submitted for genetic sequencing. Seventy-six of them (84%) have been sequenced.
Sharing
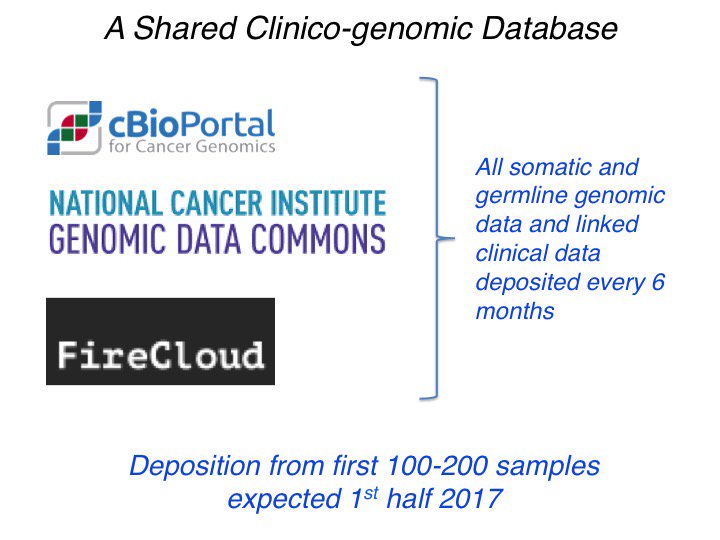
One of the main purposes of this project is to create a database that can be utilized by researchers to advance research on metastatic breast cancer. These are the sites that will be housing the MBC Project database.
Making Good On Promises
This research study is far from over. Please continue to share this work and encourage anyone with metastatic breast cancer to participate.
This research can help researchers learn why patients become resistant to certain therapies. Researchers can understand the mechanisms that are occurring in those who have extraordinary responses to treatments. With this research, we can learn the genetic differences between de novo metastatic breast cancer versus relapsed metastatic breast cancer.
Figuring out how to study cancer patients by their mutational profiles rather than by the organ where cancer arises is one goal of this research. Learning to treat patients by their mutational profiles, personalized to their mutational profiles, could be the roadmap to a cure to cancer that we all desire. It starts with the press of a button. 
**To better understand the genetics of cancer, please read our series (with videos) on Oncology Basics