Both lifestyle (the amount of sleep you get at night, amount of exercise, your levels of stress and the foods you consume) as well as genetics play a role in the development of Type 2 diabetes. People can be overweight and yet never develop Type 2 diabetes or they can be be thin and develop Type 2. A genetic predisposition is part of the equation. But the essence of this disease state is what happens to cells: a person’s own cells become resistant to the insulin that their pancreas produces.
In What is Insulin, Appreciating The Remarkable Pancreas, insulin’s action in the body is described in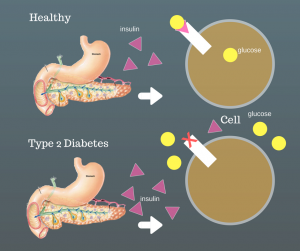 detail. Here is a snippet,
detail. Here is a snippet,
“around 5% [of the pancreas], is made up of islets of Langerhans–cell clusters containing the beta cells that create insulin…Insulin completes the digestive process–from carrots and meat to small molecules– by making it possible for cells to absorb those molecules. During digestion, amylases break down carbohydrates into glucose. That glucose enters the blood stream. Insulin is released in a bolus (large amount) from the pancreas to help the cells of the body absorb all that glucose from the blood. The cells then convert glucose into energy.”
Becoming resistant means that it takes more and more insulin to get the body’s cells to respond and absorb glucose from the blood. Unfortunately, your pancreas can only produce so much insulin. Diabetes is the result.
Reversing Type 2 Diabetes
New research looks at a dietary way to reverse type 2 diabetes. Published in the Lancet, this randomized case-control study conducted in Great Britain put patients on a formula diet of 825 to 853 calories per day for 3 to 5 months. After that period, patients were allowed (over a period 2 to 8 weeks) to gradually reinstate food and they were provided support to help them sustain their weight loss. Those in the intervention group also received cognitive behavioral therapy to help them through the process as well as tips on becoming more physically active.
 About one-quarter (23%)of the intervention group lost 33 pounds (15 kg) or more. The control group did not lose weight. Almost half (46%) of the intervention group achieved remission of their diabetes and did not need diabetes medications.
About one-quarter (23%)of the intervention group lost 33 pounds (15 kg) or more. The control group did not lose weight. Almost half (46%) of the intervention group achieved remission of their diabetes and did not need diabetes medications.
One of the features of this study was that it was conducted in family practices around Great Britain meaning that this could be accomplished with the guidance of primary care physicians. Another feature was that quality of life scores improved in the group who used the formula diet. Finally, in this study there seemed to be a link between the amount of weight loss and success in remission of diabetes, for example, 7% of those who only lost 11 pounds (5 kg) saw remission of their diabetes whereas 86% of those who lost 33 pounds (15kg) achieved remission.
These participants will be followed for four years to see how well they are able to maintain their weight loss and diabetes remission.
What do you think? Could you stay on a low-low calorie diet like the one described above? Let us know in the comments section below.






Presently, my relative has 272 count of sugar as a result of labtest. He’s so depress bec he’s also scheduled for cataract surgery but his diabetes has to be reduced to normal…We’re are so patiently doing our part for him to recovered. What more we have to do for him to be treated of his cataract and his diabetes..
I would love to try it
I would certainly be able to do this low low calorie diet with a doctor’s help and counciling. I would be very motivated knowing I could possibly reverse my type 2 Diabetes.
yes I could.
Please provide a link to the Lancet research.
ALSO, to Medivizor, please allow Twitter login to comment, not just Facebook. Many of us have turned off all all integration with FB for privacy reasons.
Hi Kathy, Thank you for catching that I had left off the link. My apologies…I’ve added it to the post but here it is again. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(17)33102-1/fulltext. Best, Kathleen
Often when I try to read a report, a pop-up box asks for email address, which I’ve provided multiple times. Then blocks further access to the article. Yes, I would like to try the T2 program. Dr. Clark
Very interesting. I’ve heard that the pancreas b-cells die off during high sugars in T2D. So, i’m pleasantly surprised to learn that the weight loss provides a remission. Wondering if the clinical trial participants were recent T2 diagnoised or the length of time of their T2. Anxiously awaiting more info. 4 months ago i got onto Jardiance along with metformin and my sugars have all been normal since. I’ve lost 18 lbs and have stayed there. I’m looking forward to finding out my new HA1C numbers!
I would welcome the opportunity to reverse my diabetes and to control the foods that I eat.This disease has my kidneys failing, heart issues and neuropathy in both my feet.. Other than that I am just fine. Oh yes I have had several congestive heart failure events. So sign me up as I would love to stay alive for my children and grandchildren
Do you have to come off insulin, metformin and gliclazide to go on this very low calorie diet
Hi Dominic,
The people in the study were not on insulin. It does appear that the intervention included removal from anti-diabetic medications. “We recruited individuals aged 20–65 years who had been diagnosed with type 2 diabetes within the past 6 years, had a body-mass index of 27–45 kg/m 2, and were not receiving insulin. The intervention comprised withdrawal of antidiabetic and antihypertensive drugs, total diet replacement (825–853 kcal/day formula diet for 3–5 months), stepped food reintroduction (2–8 weeks), and structured support for long-term weight loss maintenance.”
Importantly, they were all on the low calorie diet under physician’s supervision. That is key.
Thank you for your question. Best, Kathleen