“I had a terrible headache for two days and very seldom had headache – …once a year tops. I took my kids and Sharon to see [a] movie…and at the end…I got up…collapsed and I do not [know] what happened to me.” ~John Anderson
Stroke
Stroke is one of the most common causes of death worldwide. Although the number of deaths has gone down since 1990, the number of first and second strokes has risen; in fact in developed countries over 85% survive.
Yet there are challenges for stroke survivors. One year after stroke, 87% of survivors have a range of impairments that make resuming roles challenging. Over a third of those surviving stroke have some kind of visible disability even five years after the event. Even with rehabilitation, 42% are left dependent on others for basic care and 10% require nursing home or long-term facility care.
Although around 60% of strokes are “mild” or “minor” people who have suffered one are discharged without rehabilitation and support experience. Many people feel “deserted after discharge from hospital system…[they are] told what happens at home [is] beyond [the] stroke system purview,” Sharon Anderson believes.
John and Sharon’s Stroke Story
Before the stroke (1997), John worked as Vice President of Technology for a small tech startup.  John’s wife, Sharon, remembers, “Life was busy. [John and his co-workers] would often take the red-eye flight out of Ottawa on Wednesday night bound for California. They would attend meetings all day Thursday and Friday, fly back and then work Saturday and Sunday.”
John’s wife, Sharon, remembers, “Life was busy. [John and his co-workers] would often take the red-eye flight out of Ottawa on Wednesday night bound for California. They would attend meetings all day Thursday and Friday, fly back and then work Saturday and Sunday.”
One Sunday evening, John and the family went to a movie. As the credits rolled, John moaned and slipped down between the seats. Sharon and her 15-year-old son, Jonathan, lifted John up into a seat. “As soon as I saw him, I realized that one side of his face was drooping, so I asked Jon to go to the front, call an ambulance and tell them it was a stroke.” At the hospital, Sharon asked for tPA (Tissue plasminogen activator) the treatment that dissolves clots and improves blood flow to the brain. The doctor responded, “Those are really powerful drugs, Mrs. Anderson. We don’t do that here.” Unfortunately, though used experimentally in Canada, tPA wasn’t licensed for treatment in Canada until a month after John’s stroke.
Without the tPA, Sharon remembers, “John’s entire right side didn’t work (hemiplegia) and he had severe aphasia. He really could not communicate in any understandable way. The change from able-bodied to disabled was shocking.” Just as devastating was the news that “John’s stroke was so large, he was not a candidate for rehabilitation.”
The Importance of Rehabilitation For Stroke
“You want rehab to start quite soon and be intensive. Seven days a week if possible.” ~Sharon
Rehabilitation is crucial for people with stroke, yet there are barriers to obtaining the necessary amount for improvement. As Sharon experienced, at the hospital the focus was “deficits.”
“When I first heard the doctor use the word deficit about John, I was totally shocked–deficit to describe a person? The negativity surrounding stroke is difficult to deal with. I cannot tell you the number of times health professionals tried to ensure that we were being realistic about the chances for achieving goals. Usually, somewhere in that conversation would be a “he will never…”
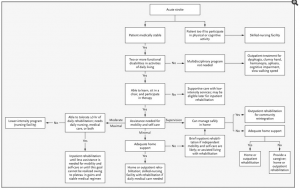
Algorithm for placement in rehabilitation care after stroke N Engl J Med. 2005 Apr 21; 352(16): 1677–1684.
Actually receiving rehabilitation is just the first step. In 1997, only around 10% of stroke patients received in-patient rehabilitation. Since then, the numbers have improved to around 25%. Sharon states, “The uncertainty about who gets rehab and when they get admitted, how long they have to wait is stressful. Many survivors are discharged, then have to wait for homecare.”
If rehabilitation is recommended, the next important piece is where you receive it. The location of rehabilitation is important to the amount of therapy received, the amount of monitoring done and the improvement achieved. According to the National Stroke Association, “Depending on the severity of the stroke, rehabilitation options can include:
- A rehabilitation unit in the hospital with inpatient therapy
- A subacute care unit
- A rehabilitation hospital with individualized inpatient therapy
- Home therapy
- Returning home with outpatient therapy
- A long-term care facility that provides therapy and skilled nursing care”
As a recent study controlled for age and extent of stroke injury reveals, location makes a difference. Comparing care at Inpatient Rehabilitation Facility to skilled nursing facility, the study finds there is greater likelihood of death and re-hospitalization if the patient is sent to a nursing home for rehabilitation instead of receiving inpatient rehabilitation.
Another factor impacting recovery is insurance. The settlement of a class action suit in 2013 prohibited Medicare from denying patients coverage for skilled nursing care, home health services, or outpatient therapy because they had reached a “plateau,” and their conditions were not improving.
Yet stories of denial of rehabilitation or extremely short allowance for rehabilitation by health insurance companies abound. In one example, United Healthcare, denied requests for rehabilitation for Brett Walls, even though his doctors saw progress and believed improvements would continue from rehabilitation at an intensive rehab facility. In one write-up about this case, his wife Gail asks,
“Why should you have to fight? Why should you have to get the media involved? Why do you have to get all over their Twitter and Facebook page? Why? Why? Why? Why? They just rubber stamp, rubber stamp, rubber stamp, rubber stamp, hoping you give up.”
In Canada, Sharon relates, “if you don’t follow the path exactly as system dictates you have a difficult time getting rehab. For example, a mild stroke survivor here in Alberta can be referred for six weeks of therapy by home rehab team, but they have to have that referral before they leave hospital. They can’t get it from family doctor after.”
John’s Stroke Experience
 When John awoke in the hospital he says, “I thought I could go back to work …I did not understand my problem even in the hospital.” While sitting in a wheelchair, he thought he could get up and walk away. He thought that he was understanding and speaking perfectly, “but I would say ‘yes’ to every question.” He remembers, “It took about two or three years to get out of the fuzzy physical/mental problem.”
When John awoke in the hospital he says, “I thought I could go back to work …I did not understand my problem even in the hospital.” While sitting in a wheelchair, he thought he could get up and walk away. He thought that he was understanding and speaking perfectly, “but I would say ‘yes’ to every question.” He remembers, “It took about two or three years to get out of the fuzzy physical/mental problem.”
Sharon believes that John was lucky. “The young physio[therapist] who had been working with him in acute care…phoned me at home and explained that…he wasn’t a candidate for in-patient rehab, but she thought he had potential. She recommended that I take him home and hire private therapists if we could afford it.”
Not wanting her 11 and 15 year old to see their father in a nursing home, Sharon found a service that would work with John. They even succeeded in getting John admitted to an in-patient rehabilitation facility. After four months “he could walk a few steps and say a couple of words.”
“Rehab can do wonders,” Sharon believes. Even so, there is little support of rehabilitation. “Less than 5% of stroke research budgets are spent on rehabilitation.”
So, there are still so many misconceptions about recovery and neuroplasticity. There is a myth that people with stroke plateau at six months even with rehabilitation. Efforts at recovery shouldn’t be limited to the first six months. Our adult brains are capable of forming new pathways and it is worth the effort to provide opportunities for that growth.
Caregiving Versus Relationship
Sharon is a trained dental hygienist and has been in practice throughout. “When John could manage kids and house,” she went back to school and is now completing her PhD in Human Ecology at the University of Alberta. Prior to this she completed a Masters in Community Rehabilitation at the University of Calgary and a Masters in Health Promotion at the University of Alberta.
“It has been good, John and I have learned from each other.”
“John has taken over family management and runs his website. I do university stuff. We collaborate as most couples do.”
Their experience has fueled Sharon’s academic work. She believes that “Stroke research is underfunded, stroke rehab particularly so! With [so much] emphasis on awareness, what happens after discharge [is] overlooked.”
She’s published several articles, made numerous presentations and is conducting research on spouses of stroke survivors. “Currently, we think of spouses only as caregivers– but what both survivors and spouses want is a relationship….Maybe like deficit, we need to find a different word than caregiver. It really makes the survivor into an object of care.” Both people lose personhood and in that loss of personhood, they lose relationship.
Impairment From Stroke Versus Adaptation
Sharon feels that the emphasis on impairment clouds the prospect of adaptation. “There has to be a better way to deal with stroke over the long term. Illness and disability are part of life.” With 85% of people surviving stroke, but without the support and services after hospital discharge, “Families are left to their own devices. How do we ensure that people live that life as fully as possible?”
“In the medical focus on cure, I…think living life is overlooked.”
*Based on email correspondence with John and Sharon Anderson May 2015 and on #HCHLITSS Tweetchat






