Around one million people in the US have Parkinson’s disease. In Parkinson’s, the dopamine-producing cells of the brain–in an area called the substantia nigra–die off.
Abnormal proteins are what kill these brain cells. In fact, all neurodegenerative diseases have deposits of abnormal proteins, and neurobiologists call them “protein-opathies,” Paul Fishman, MD PhD professor of neurology at the University of Maryland School of Medicine told an online and in person audience.
“We are born with all of the brain cells we ever have. For certain populations of cells with fixed numbers, when you lose them, you have neurological symptoms,” Dr. Fishman explained.
When the brain loses cells in Parkinson’s disease, there is a cascade of cells that become overactive, specifically in the region of the subthalamic and globus pallidus, Dr. Fishman said. This part of the mid-brain has a significant role in controlling movement. The dopamine produced here moves throughout the brain, affecting areas involved in learning and emotion. Hence, Parkinson’s disease is a movement disorder and over time, can include a form of dementia.
Treatment for Advanced Parkinson’s Disease
Reducing symptoms by replacing dopamine is the first line of treatment and can be effective for a number of years. As the disease progresses, “on-time” – the time when dopamine medication works effectively – becomes shorter and shorter. “In early Parkinson’s, it [dopamine medication] seems to work as a long-acting medication, but for advanced Parkinson’s, [dopamine medication] acts as what it is, a short-acting medication…eventually acting inconsistently and erratically,” Dr. Fishman said. When the disease progresses to this point, patients look to surgery for symptom relief.
Prior to Deep Brain Stimulation, DBS, as a treatment option, neurologists did “lesion surgery”- a type of surgery that destroys part of the brain. “When you are talking to a patient, it is totally counterintuitive that you can improve part of their disease by killing part of their brain. The problem with their brain is that they are losing cells. Why would you get better killing more of them?” Dr. Fishman said. Yet in a certain percentage of people, lesion surgery worked.
For many years now, Deep Brain Stimulation or DBS has been the treatment option of choice to improve patient’s on-time, reducing their off-time and effectively reducing tremors. Over 170,000 of these surgeries have been conducted in the US.
Yet, according to Dr. Fishman, even though people experience benefits from DBS, there are risks. First, the patient must undergo two surgeries. Second, a surgeon inserts a probe in the brain to identify the location of the implant, potentially damaging the brain. Third, infection and hemorrhaging may also occur. Because of these risk factors, Dr. Fishman has been researching other, less invasive surgeries.
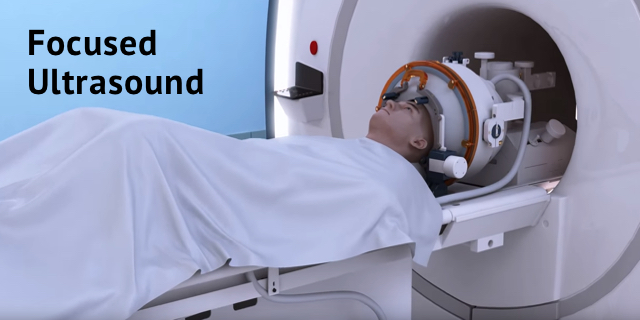
Focused Ultrasound (FUS), DBS and the Blood Brain Barrier
Dr. Fishman is involved in using focused ultrasound or FUS. FUS utilizes the experience of lesion surgery but without cutting into the skull or brain. With MRI-guided focused ultrasound (MRgFUS), neurologists destroy overactive brain centers.
The patient is awake during the procedure. “As we apply sonic energy, we give it in a dose titration, just like giving a drug…we observe the patient, see that everything is good …give a dose escalation. And we do it in real time,” said Dr. Fishman.
MRI monitors local brain temperature after each sonic treatment raising the brain temperature in the problem area slowly. As the patient experiences symptom relief, the neurologist confirms the target. “The patient confirms optimal clinical results.”
Dr. Fishman and his colleagues have also discovered a feature of FUS that is very exciting. When applied to the blood brain barrier, sonic energy produces openings that can be used to get larger molecules like antibodies or even stem cells into the brain. Once these larger treatment entities are in the brain, the researchers are working to assure that they go to the right location in the brain to treat the condition. Using magnets and stem cells packed full of nanoparticles infused with iron, research in animals is getting stem cells to the areas of the brain where regeneration of cells is needed.
Webinar
To learn more and hear Dr. Fishman speak, join the Michael J. Fox Foundation Third Thursday Webinar “Beyond Medication: Deep Brain Stimulation and Focused Ultrasound for Parkinson’s” on Thursday, February 21, 2019, 12 to 1 p.m. ET
To learn more about Parkinson’s disease and new research being done, sign up for Medivizor.