

Title of notification
A personalized refresher about infertility & reproductive technologies
What is infertility?
Infertility, or the inability to conceive, affects 5-15% of couples worldwide. The exact definition of infertility varies around the world. In the united states, infertility is defined as failure of a couple to conceive after 12 months of timed (with ovulation), unprotected intercourse in women younger than 35 years of age, and after six months in women 35 years and older.
Fertility of a couple is usually discussed in terms of fecundability. Fecundability refers to the probability of conception in one menstrual cycle. It is believed that the chances of conception (in fertile couples) in one random intercourse is about 0.15, and following frequent unprotected intercourse (not timed with ovulation) it is 0.25. However, fecundability decreases over time, so conception is most likely in the first few months of unprotected intercourse. About 60% of the couples will conceive within 6 months of frequent intercourse, after 12 months about 85% and after 18 months – 90% of couples will conceive successfully.
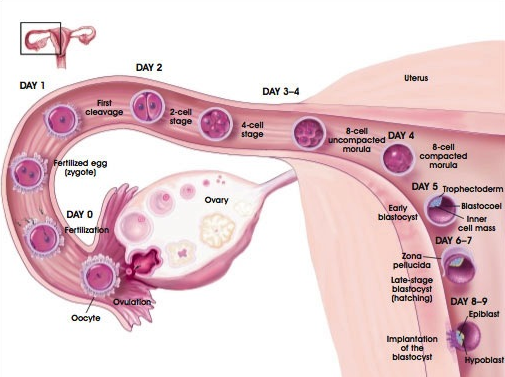
Fertilization and conception: understanding the process
The reasons for infertility
The ability of a couple to become pregnant depends on normal fertility in both the male and female partners.
Among all cases of infertility in developed countries, about a third can be traced to each - male, female and unexplained infertility (a cause cannot be determined).
Multiple risk factors for infertility have been identified, common for both male and female.
These include age, smoking, obesity, low body weight and eating disorders, alcohol consumption,diabetes and a sedentary life style.
Reasons for female infertility
For pregnancy to occur, a woman must ovulate (produce and release eggs) regularly, have timed intercourse with a fertile partner (or timed insemination with an intact sperm), and have an intact genital system (normal fallopian tubes, uterus and cervix).
At times, conception occurs, but the body is unable to carry the fetus to full term, and miscarriage ensues. Inability to conceive following a previous miscarriage or stillbirth is often referred to as secondary infertility.
Miscarriage, stillbirth and secondary infertility
Miscarriage is the spontaneous loss of a pregnancy before the 20th week; 80% of these occur in the first 12 weeks. About 10%-20% of reported pregnancies end in a miscarriage. Known risk factors for spontaneous abortion are advanced maternal age, previous miscarriage(s), and maternal smoking.
Miscarriage happens because something was amiss in the carrying of the pregnancy. Most miscarriages occur because the fetus isn't developing normally. However, it is often difficult to determine the cause.
Miscarriage is most commonly (up to 90%) caused by chromosomal abnormalities in the egg. These most often lead to an early pregnancy loss (before the 12th or even 8th week). Exposure to teratogens may also cause early pregnancy losses, although to a lesser extent.
In some cases, medical conditions in the pregnant woman, such as uncontrolled diabetes, genital infections or structural problems in the reproductive tract, such as uterine fibroids, can lead to miscarriage. Some autoimmune diseases are commonly implicated as a cause of miscarriage. Thrombophilia may lead to the formation of obstructive blood clots in the placenta. This often leads to late miscarriages (at the second or third trimesters) or stillbirth.
When a fetus is lost later in the course of the pregnancy, after the 23rd week, the condition is referred to as a stillbirth. Causes of stillbirths may include infections and trauma, as well as growth retardation, thrombophilia and preeclampsia.
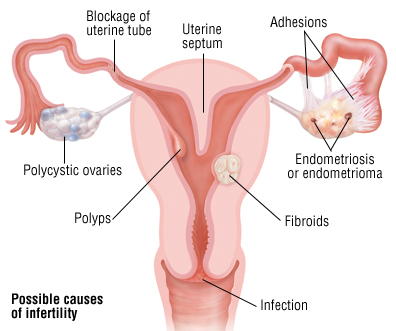
Common causes of female infertility
Ovulation disorders
Ovulation disorders disrupt the processes of egg production and/or release. It is estimated that 25% of female infertility is caused by ovulation disorders. Examples of conditions that interfere with ovulation include polycystic ovary syndrome (PCOS), excessive exercise, eating disorders, and ovarian tumors. Hormonal disorders such as hyperthyroidism or hypothyroidism, and hyperprolactinemia can also interrupt the menstrual cycle and cause infertility. Premature ovarian failure, also called early menopause, occurs when menstruation and ovulation end before the age of 40. Although the cause of early menopause is often unknown, certain conditions such as autoimmune diseases and cancer treatments may cause ovarian failure.
Endometriosis
Endometriosis is a condition in which endometrial tissue (cells of the inner-most layer of the uterus which grow in response to hormonal stimulation and sheds during menstruation) implants and grows outside of the uterus. Endometriosis most commonly involves the ovaries, bowel or the tissue lining the pelvis. Rarely, endometrial tissue may spread beyond the pelvic region. This added growth of hormone responsive tissue affects the function of the ovaries, uterus and fallopian tubes, and is a common cause of female infertility. Endometriosis is estimated to be the cause of female infertility in 15% of the cases.
Pelvic adhesions
Pelvic adhesions (or scar tissue) are a common cause of infertility. Adhesions are areas of fibrous tissue that form as a result of the healing process which remain after the original inflammation or trauma has healed. Adhesions can cause different reproductive organs in the pelvis to become stuck together. As a result, adhesions can distort the normal pelvic anatomy or cause decreased mobility and function. Pelvic adhesions can result from a number of different causes. Common causes of adhesions are infections, previous surgery, abdominal trauma, endometriosis , and appendicitis.
Fallopian tube damage or blockage
Fallopian tube damage or blockage can prevent travel of the egg after ovulation, interrupting both fertilization of the egg, and implantation in the uterus. Damage to the fallopian tubes commonly results from inflammation. Salpingitis and pelvic inflammatory disease are common results of sexually transmitted infections, such as Chlamydia or Gonorrhea. Adhesions (internal scarring) around the fallopian tubes are another common cause of blockage. Adhesions are frequent complications of pelvic surgery or infections. Tubal blockage or abnormalities are estimated to be the cause of 30-35% of female infertility.
Uterine or cervical abnormalities
Uterine or cervical abnormalities can prevent both fertilization and implantation of the egg. Inability of the cervix to produce normal mucus (called ‘hostile mucus’), as well as inborn anomalies and trauma to the cervix or uterus (including surgery) may impair fertility. Genetic disorders are a common cause of these abnormalities. The wall of the uterus is also a common site of tumors in women (such as fibroids). Most tumors are benign (not cancerous), however even these can distort the uterine cavity and interfere with implantation of the fertilized egg. Uterine growths and anomalies (such as septate uterus) will most likely lead to repeated miscarriages (due to placental dysfunction) rather than failure to conceive.
Chromosomal abnormalities and genetic mutations
Chromosomal abnormalities and genetic mutations may be the cause of both male and female infertility. Mutations in genes responsible for the production of hormones or their receptors may lead to abnormal ovulation or fetal development. Chromosomal abnormalities of the female sex chromosome, the X chromosome, such as Turner syndrome may also be the cause of infertility.
Medications
Medications may be the cause of reduced fertility, and in most cases normal fertility is restored when the medication is stopped. Commonly used medications that may cause infertility include chemotherapy agents used to treat cancer, drugs used in the treatment of immune diseases such as colchicine and sulphasalazine, steroids, NSAIDs (non steroidal anti-inflammatory drugs) such as aspirin or ibuprofen, and diltiazem (a common drug used in the treatment of cardiovascular conditions).
Reasons for male infertility
Conception requires the production of functional sperm and seminal fluid (the semen’s plasma), transport of the semen through intact sperm ducts, and a normal ejaculation mechanism. The male sperm must then successfully travel the female’s cervix, reach the fallopian tube and fertilize the ovulated egg.
Watch this video about normal fertilization and conception (02:00)
The common causes of male infertility are listed below, however, 40% to 50% of male infertility are of unknown cause.
Abnormal production or function of sperm
Abnormal production or function of sperm is a leading cause of male infertility. Any factor that affects the number or shape of the sperm produced can lead to male infertility. These include inborn genetic defects, undescended testis, or infections which affect the testis, such as mumps. Overexposure to certain environmental factors, such as pesticides, radiation, or frequent exposure to heat (such as frequent visits to saunas or hot tubs), can severely impair sperm production. Enlarged veins in the testis (called varicocele) are a common problem that increases blood flow to the testis thereby producing excessive heat.
Endocrine conditions
Endocrine conditions, or hormonal imbalances, affect both male and female fertility.In men, the production of sperm is dependent on proper hormonal stimulation. Therefore, conditions such as thyroid dysfunction and hyperprolactinemia may be the cause male infertility.
Problems with sperm delivery
Chromosomal abnormalities and genetic mutations
Chromosomal abnormalities and genetic mutations may be the cause of both male and female infertility. Chromosomal abnormalities in the male sex chromosome, the Y chromosome, such as Klinefelter syndrome, may be the cause of male infertility. Inherited mutations in genes associated with cystic fibrosis (CF) can also result in male infertility due to a low sperm count or obstructed sperm ducts. Recently, mutations in the gene responsible for the production of androgen receptors have been implicated as a possible cause of male infertility.
Cancer
Evaluation and diagnosis of infertility
Several changes in lifestyle and sexual habits may improve the chances of conceiving, and it may be worthwhile to investigate these before starting a complete medical evaluation.
General recommendations state that the evaluation of infertility should not be considered unless a couple has been trying to conceive regularly for at least one year. Women aged 35 to 40 may wish to contact their physician earlier if they have been unable to conceive for six months or longer. Women over the age of 40, or those with irregular, absent or painful menses, should contact their physician to begin evaluation and treatment as soon as they consider conceiving. This is also true if any of the partners has known fertility problems or has received cancer treatments in the past.
Because pregnancy requires normal fertility in both the male and female, healthcare providers routinely involve both partners in the evaluation.
Infertility workup usually begins with a medical history, a thorough physical examination, semen analysis and some preliminary lab tests done by a gynecologist or fertility specialist. The past health and medical history of both men and women may provide some clues about the cause of infertility. In particular, the menstrual history (i.e. whether a woman has monthly, regular periods) may reveal ovulatory problems.
Blood tests can provide information about the levels of several hormones that play a role in female and male fertility. In women, these hormones mainly include follicle-stimulating hormone (FSH) to assess how well the ovaries are functioning, TSH to test thyroid function, and prolactin to assess the possibility of a pituitary tumor. In men with a suspected hormonal problem (i.e. with a low sperm count) hormones assessed include testosterone, luteinizing hormone (LH), FSH and prolactin.
Another component in the basic evaluation of infertility is the assessment of the female fallopian tubes and uterus (in order to detect defects or blockages) using imaging studies such as hysterosalpingography (HSG), hysteroscopy, ultrasonography (US) and laparoscopy.
Medical tests and treatment trial periods may extend over a period of several months. The process is emotionally stressful for many couples, and in some cases no cause is found even after extensive testing.
Evaluation of infertility in women
Evaluation of infertility in women begins with a general history and physical examination to look for risk factors or obvious reasons for infertility. This includes a detailed questioner regarding the menstrual history (cycle length and characteristics), sexual habits and frequency of intercourse, any prior infections or surgeries, a family history regarding pregnancies, births and miscarriages, and an evaluation of smoking, drug use and drinking habits. The physical examination will include a standard gynecological exam.
Specific fertility tests for women may include the following:
Ovulation testing
Determining whether or not a woman is ovulating is the corner stone of female fertility evaluation. A simple blood test, measuring the levels of the hormone progesterone, is performed approximately one week before the expected menses (on day 21 of the menstrual cycle). A progesterone level higher than 3 ng/mL is evidence of recent ovulation. Urine test kits are often sold over the counter, and can reliably detect ovulation. These kits detect a surge in the levels of a hormone called luteinizing hormone (LH), which acts as a trigger for female ovulation.
Hormonal regulation of the menstrual cycle
The menstrual cycle is the monthly series of changes a woman's body goes through in preparation for the possibility of pregnancy. Each month, one of the ovaries releases an egg - a process called ovulation, leaving a ruptured follicle (the sac that contains each egg) behind. The ovulation process begins in day 1 of the cycle (first day of period), when a follicle begins to develop in the ovary. Follicular stimulating hormone (FSH) provides the necessary stimulation for the follicle's maturation. Around day 14 of the cycle, a peak in the levels of luteinizing hormone (LH) stimulates the follicle to release the egg. The now empty follicle begins to release progesterone, which stimulates the innermost lining of the uterus (the endometrium) to grow in anticipation of an embryo. If the egg isn’t fertilized and implanted in the uterus, progesterone levels drop and menses occurs as the new endometrial tissue is shed through the vagina. This is a menstrual period.
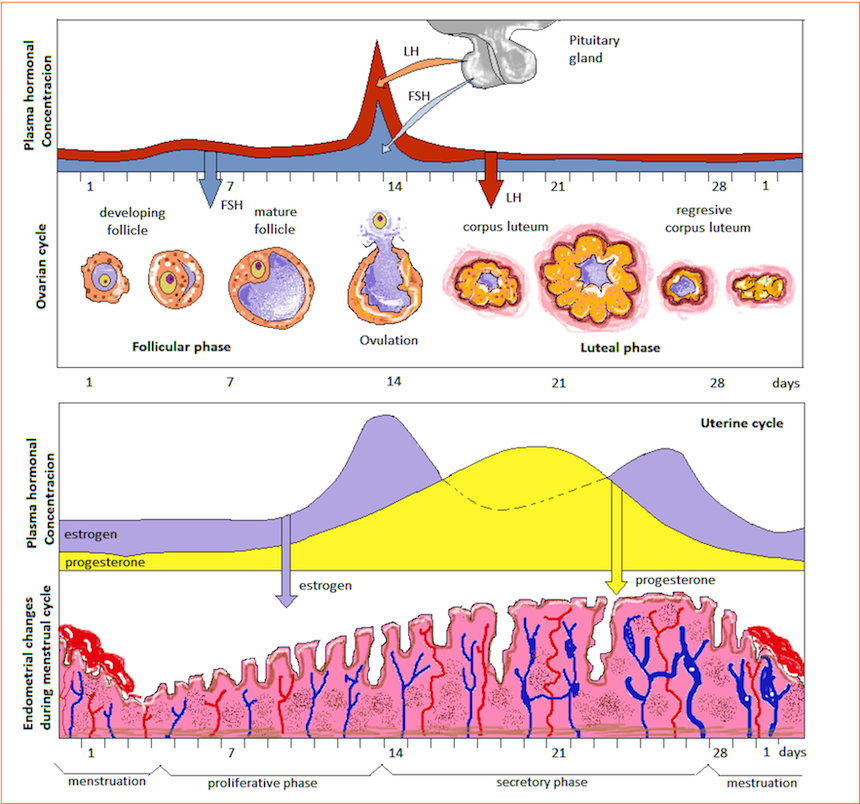
Assessment of ovarian reserve
The ovaries store a limited amount of viable eggs, and a single mature egg ready for fertilization is released every month during ovulation. Examining the quality and number of eggs available for ovulation (called the ovarian reserve) is also an important step in the assessment of female infertility. Assessment of ovarian reserve is usually preformed by measuring the levels of certain hormones (by a blood test) during the early days of the menstrual cycle. The most common test in use is the day 3 FSH test. This exam measures the levels of follicle stimulating hormone on the 3rd day of the menstrual cycle.
Ultrasound (US) imaging can also be used to determine the number of antral follicles found in the ovaries. This exam is referred to as antral follicular count (AFC), and the image of the ovaries is obtained by transvaginal US.
Although FSH, and more recently Inhibin B, have been shown to predict ovarian reserve, it is now well established that Anti-Mullerian Hormone (AMH) is a more useful test. High levels, however, can be present in women with Polycystic ovarian syndrome (PCOS) which compromises female fertility, and therefore a combination of AMH and a transvaginal ultrasound to count the number of antral follicles is probably the best way to assess ovarian reserve and future fertility. This combination is sometimes referred to as the Biological Body Clock Test.
Further hormone testing
The levels of other hormones are also frequently tested in the evaluation of infertility. These include thyroid and pituitary hormones that affect the reproductive system, such as prolactin, thyroid stimulating hormone (TSH), and screening for polycystic ovary syndrome (PCOS) (imbalanced hormones suggestive of the syndrome, for example elevated testosterone in the bloodstream).
Laparoscopy
If the results of the imaging studies are inconclusive, or if adhesions or endometriosis are suspected, a diagnostic laparoscopy may be recommended. This minimally invasive procedure entails insertion of a small camera through an incision below the naval. A laparoscopy allows surgeons to look at a woman's reproductive organs, including the uterus, ovaries and fallopian tubes. Any blockages, scarring, adhesions or irregularities can be identified and sometimes treated on site.
Genetic testing
Genetic testing may be recommended if there is a suspicion that genetic or chromosomal abnormalities are contributing to infertility. These tests usually require a small blood sample, which is sent to a laboratory for evaluation.
In women, abnormalities of the female X chromosome are examined. In Turner syndrome for example all or parts of one X chromosome are missing.
Although infertility treatments may be able to overcome genetic or chromosomal abnormalities, there is a possibility of transferring the abnormality to a child. In this case, genetic counseling is often recommended to inform the couple about the possibility of parent-to-child transmission and the possible impact of the abnormality.
Evaluation of infertility in men
Evaluation of infertility in men begins with a general history and physical examination to look for risk factors or obvious reasons for infertility. This includes a detailed questioner regarding the age of puberty, sexual function and habits, sex drive, frequency of intercourse, any prior infections or surgeries, and an evaluation of smoking, drug use and drinking habits. The physical examination will include a thorough examination of the genitals by an urologist or fertility specialist.
Specific fertility tests for men may include the following:
Semen analysis
Semen is usually obtained by masturbation and ejaculation into a container. In the lab semen is analyzed to determine the amount, shape and motility (the movement and travel ability) of the sperm. The seminal fluid is also analyzed since low seminal fluid volume, high viscosity or changes in acidity may also be a cause of infertility.
According to the World Health Organization (WHO), a normal sperm count varies from 15 to 150 million sperm per milliliter. The normal volume varies from 1.5 to 5.0 milliliter per ejaculation. At least 58% of the sperm cells should be vital (alive and functional), and at least 40% should be motile and show normal forward movement. At least 50% of sperm cells should display normal morphology (shape) based on the WHO. According to the Kruger's Strict criteria (an updated way of determining sperm shape) only 4% suffice.
Hormonal testing or endocrine assessment
A blood test to determine the levels of male hormones is a simple procedure that may provide important information regarding male fertility. Endocrine assessment includes measurements of three main hormones: testosterone, LH, and FSH. Since these three hormones affect the production of one another through a complicated feedback system, comparison of their relative levels may pinpoint the cause of infertility.
Ultrasound (US)
US imaging of the testicular scrotum can identify anatomical abnormalities and obstructions in the testicles and supporting structures.
If a blockage in the sperm ducts (epididymis or vas deferens) is suspected, a transrectal US may be ordered. A transrectal US also allows the doctor to check the prostate gland, and seminal vesicles.
Genetic testing
Genetic testing may be recommended if there is a suspicion that genetic or chromosomal abnormalities are contributing to infertility. These tests usually require a small blood sample, which is sent to a laboratory for evaluation.
In men, chromosomes are examined for subtle changes in the male sex chromosome, the Y chromosome. Chromosomal abnormalities such as Klinefelter syndrome, and inherited mutations in genes associated with cystic fibrosis (CF) may be found as the cause of infertility after genetic testing.
Although infertility treatments may be able to overcome genetic or chromosomal abnormalities, there is a possibility of transferring the abnormality to a child. In this case, genetic counseling is often recommended to inform the couple about the possibility of parent-to-child transmission and the possible impact of the abnormality.
Other tests
A testicular biopsy may be recommended in men with no sperm found in the semen analysis. The biopsy allows the physician to determine whether sperm is produced in the testis. The presence of sperm in the testis when there are none in the ejaculate suggests blockage along the sperm ducts.
Post-ejaculation urinalysis is performed if retrograde ejaculation is suspected. A urine sample is taken after ejaculation to test for sperm cells in the urine.
Anti-sperm antibody tests are performed to determine if immunity against sperm cells exists. These tests check for immune cells (antibodies) that attack sperm. Men who had a vasectomy reversal are likely to have anti-sperm antibodies.
Specialized sperm function tests . A number of tests can be used to check how well the sperm survive after ejaculation, how well they can penetrate an egg, and whether there is any problem attaching to the egg.
Fertility treatments and reproductive technologies
Once the cause of infertility is identified, therapy aimed at correcting reversible causes can be started. In some cases, the cause of infertility cannot be corrected. Technological advancements may allow for conception even if the cause of infertility is irreversible. However, these treatments involve a significant physical, psychological and financial commitment.
Lifestyle and habit modifications to improve fertility
Most causes of infertility require medical treatment, however, several strategies and changes in lifestyle may increase fertility and improve the chances of pregnancy.
Regular, frequent, intercourse several days before and until a day after ovulation offers the highest chance of pregnancy. Ovulation occurs at the middle of the menstrual cycle, halfway between periods. Home kits are available which can predict the time of ovulation.
Drugs and tobacco, as well as excessive alcohol consumption are known to reduce fertility, and should be avoided. Men should take care to avoid hot temperatures such as regular hot-tub and steam bath use. Women should maintain normal body weight, since both overweight and underweight women are known to be at a higher risk for ovulation disorders. Moderate exercise may improve fertility, but intense exercise should be avoided.
Before starting treatment
Infertility treatments can be a long and exhausting process. There are no guaranties regarding the length of treatments, their overall cost or the final outcome. Fertility treatments may be very expensive, are often not covered by insurance, and successful conception often requires repeated attempts.
Couples should make sure they are fully prepared for this difficult and stressful course. Couples should make sure they are fully informed regarding the exact nature and effect of the treatments they are about to receive. Setting limits and deciding in advance how many and which types of procedures to receive can help in coping with this emotionally stressful process. Couples may also wish to consider other options of fertility treatment. Alternatives such as adoption, donor sperm or surrogacy should be discussed as well before deciding on a course of treatment.
Social support is important in enduring the long process of fertility treatments. Couples should consider joining support groups or regular counseling to help express frustrations and anger, reduce stress, and prepare for the eventuality that treatments may fail.
Medical treatments for infertility
The treatment for female infertility depends on the medical problem causing infertility.
Ovulation disorders can usually be treated by ovulation induction (stimulating ovulation using fertility drugs). Commonly prescribed drugs used to induce ovulation include clomiphene (Clomid) and gonadotropins (Repronex or Follistim). If needed, after ovulation is induced eggs can harvested for IVF, or preserved with cryopreservation for future use. If a low ovarian reserve or complete ovulation failure is the cause of infertility, IVF using egg donation may be considered.
Cervical abnormalities that lead to infertility are best treated by bypassing the abnormal cervix. IUI usually offers good chances of conception.
Uterine abnormalities that prevent a normal pregnancy can sometimes be corrected by surgery. However, in many cases surrogacy should be considered.
Fallopian tube obstructions may be repaired surgically. At times, IVF is recommended for such women due to old age or severe damage of the fallopian tubes.
Endometriosis and other abnormal uterine growths, such as polyps, myomas or scar tissue, can be treated with surgery. Once these factors are removed ovulation induction and IUI or IVF may still be performed if necessary.
Male infertility can be overcome by the treatment of general sexual dysfunctions, such as impotence or premature ejaculation. If inability to ejaculate is a factor (such as in the case of spinal cord injuries), sperm can be retrieved with surgical aspiration (extraction with a needle). This procedure is referred to as percutaneous epididymal sperm aspiration (PESA). Other procedures, such as testicular sperm extraction (TESE) and microsurgical epididymal sperm aspiration (MESA), are similar sperm retrieval methods employing slightly different techniques. If semen analysis is abnormal, extracted sperm from the male partner can be delivered into the uterus by intrauterine insemination (IUI), or injected directly into the female egg in the lab by a procedure called intracytoplasmic sperm injection (ICSI) as part of in-vitro fertilization (IVF). Sperm retrieved from the testis may also be preserved through cryopreservation for future use if needed. If sperm production is severely impaired, sperm donation may be considered. Drug treatments may also be prescribed for hormonal disorders causing infertility, such as prolactin-secreting tumors or hypogonadism. Hormonal treatments such as luteinizing hormone analogs, testosterone and follicular stimulating hormone analogs may be used to enhance sperm production and viability.
Assisted reproductive technology (ART)
ART refers to any treatment in which the female egg, the male sperm, or both are handled, and pregnancy is achieved in an artificial manner. The exact treatment of infertility depends on the cause found. Treatments may include drug therapy (infertility medications), surgery, and procedures such as intrauterine insemination, intracytoplasmic sperm injection (ICSI).
In-Vitro Fertilization (IVF) is the most common form of assisted reproductive technology, and offers the highest chance of conception for most couples. IVF involves harvesting mature eggs from the female, fertilizing the eggs with the male's sperm in a lab dish, and then implanting the fertilized eggs into the uterus lining three to five days after fertilization. Several techniques can be used during IVF to increase the chances of treatment success.
Intracytoplasmic sperm injection (ICSI) is a method of fertilization often performed as part of IVF. ICSI includes injection of treated sperm (from the male partner or a donor) directly into the egg (from the female partner or a donor). ICSI has been found to increase the success rate of IVF.
Watch this video about in-vitro fertilization (00:59)
Intra-Uterine Insemination (IUI)
IUI is a simple, low cost, procedure that is often used when cervical abnormalities or abnormal sperm production is the cause of infertility. Sperm is collected from the male partner and is then washed (a critical step as the semen contains a substance called prostaglandin, which contracts the uterus and may cause rejection of the fertilized egg) concentrated, and placed directly in the uterus around the time of ovulation. IUI is often used in conjunction with fertility drugs. When donor sperm is used for insemination this process if often referred to as artificial insemination by donor (AID).
Watch this video about intra-uterine insemination (00:29)
Complications of infertility treatments
Multiple pregnancies is the most common complication of infertility treatments. Since treatments are expensive, and pregnancy is not always achieved, multiple fertilized eggs are implanted during IVF to increase the chances of success. This also raises the chance for multiple fetuses (twins, triplets or more). Multiple fetuses dramatically increase the risk of premature labor, low birth weight and developmental problems.
Infertility treatments may cause several other unwanted complications. Ovarian hyperstimulation syndrome (OHSS), in which the ovaries become swollen and painful, may result from several fertility drugs used in ovulation induction. Signs and symptoms of OHSS may include abdominal pain, shortness of breath, bloating, nausea and kidney failure. A possible risk in this condition is torsion of the involved ovary. Ovarian torsion is the partial or complete rotation of the ovary (often together with its fallopian tube) around its ligament, resulting in a compromise to the blood supply to it. This is a gynecological emergency as any delay will result in death of ovarian tissue, which will result in subfertility.
s sperm in a lab dish, and then implanting the fertilized eggs into the uterus lining three to five days after fertilization.'>in-vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI).In-Vitro Fertilization (IVF) is the most common form of assisted reproductive technology, and offers the highest chance of conception for most couples. IVF involves harvesting mature eggs from the female, fertilizing the eggs with the male's sperm in a lab dish, and then implanting the fertilized eggs into the uterus lining three to five days after fertilization. Several techniques can be used during IVF to increase the chances of treatment success.
Intracytoplasmic sperm injection (ICSI) is a method of fertilization often performed as part of IVF. ICSI includes injection of treated sperm (from the male partner or a donor) directly into the egg (from the female partner or a donor). ICSI has been found to increase the success rate of IVF.
Watch this video about in-vitro fertilization (00:59)
Intra-Uterine Insemination (IUI)
IUI is a simple, low cost, procedure that is often used when cervical abnormalities or abnormal sperm production is the cause of infertility. Sperm is collected from the male partner and is then washed (a critical step as the semen contains a substance called prostaglandin, which contracts the uterus and may cause rejection of the fertilized egg) concentrated, and placed directly in the uterus around the time of ovulation. IUI is often used in conjunction with fertility drugs. When donor sperm is used for insemination this process if often referred to as artificial insemination by donor (AID).
Watch this video about intra-uterine insemination (00:29)
Complications of infertility treatments
Multiple pregnancies is the most common complication of infertility treatments. Since treatments are expensive, and pregnancy is not always achieved, multiple fertilized eggs are implanted during IVF to increase the chances of success. This also raises the chance for multiple fetuses (twins, triplets or more). Multiple fetuses dramatically increase the risk of premature labor, low birth weight and developmental problems.
Infertility treatments may cause several other unwanted complications. Ovarian hyperstimulation syndrome (OHSS), in which the ovaries become swollen and painful, may result from several fertility drugs used in ovulation induction. Signs and symptoms of OHSS may include abdominal pain, shortness of breath, bloating, nausea and kidney failure. A possible risk in this condition is torsion of the involved ovary. Ovarian torsion is the partial or complete rotation of the ovary (often together with its fallopian tube) around its ligament, resulting in a compromise to the blood supply to it. This is a gynecological emergency as any delay will result in death of ovarian tissue, which will result in subfertility.
Treatment of unexplained infertility
While the cause of unexplained infertility is unknown, it is probably due to subtle functional abnormalities in ovarian, sperm or uterine function. The management of couples with unexplained infertility may include the same therapies and interventions as explained fertility, such as ovulation induction, IUI or IVF.
Therapy is usually started with treatments that are low risk and of low cost such as lifestyle changes. Treatments of greater risks and cost, such as ovulation induction, IUI or IVF are tried sequentially if earlier treatments fail to achieve pregnancy. The success rate of IVF in couples with unexplained infertility is significantly smaller compared to IVF treatments in couples with a known cause of infertility. However, IVF still offers the highest pregnancy rate in the shortest time for these couples.
Cutting-edge research on fertility and reproductive techniques
Home kits for the assessment of ovulation by a urine test have been sold over the counter in many countries. Recently, new at-home tests for the evaluation of infertility have become available for couples trying to conceive. An over the counter test for evaluating sperm quality is now also commercially available. This test provides an estimate of the total number of motile sperm. However, since this test is relatively new, only limited data is available regarding the accuracy and reliability of this test.
Germ cell transplantation is an exciting prospect in the treatment of male infertility. Germ cells have the ability to differentiate and mature into a wide variety of functional cells, including sperm cells. In preclinical rodent studies, germ cells from the testis of healthy mice were transplanted into the testis of infertile mice. Normal sperm cell production and pregnancy was achieved after successful mating of the treated mice with female mice. These trials suggest that germ cell transplantation may become a treatment for male infertility due to genetic diseases or damage of the reproductive system due to cancer treatments.
Newly introduced strategies for ovulation induction are also the focus of recent research. Insulin sensitizers such as metformin (Glucophage) are commonly used in the treatment of infertility caused by PCOS. Results of recent trials suggest that insulin sensitizers may also assist in improving ovulation, and the possibility of adding these drugs to standard ovulation induction is now under review. However, currently such treatment is not recommended due to insufficient evidence.
Aromatase inhibitors, such as letrozole (Femara), have also recently been found beneficial as an alternative to standard ovulation induction with clomiphene. Aromatase inhibitors lead to the release of fewer eggs, thereby decreasing the risk of multiple pregnancies. The combination of aromatase inhibitors with gonadotropins appears to be especially promising. However, data regarding the use of aromatase inhibitors as ovulation induction drugs is limited, and the US Food and Drug Administration (FDA) has not yet approved the use of aromatase inhibitors for this indication.
Other possible future developments in the treatment and prevention of infertility include diagnostic methods for causes of infertility in early adulthood, preventing infertility with early diagnosis and treatment of sexually transmitted infections, and identification of environmental toxins that may be the cause of infertility.
Finally, most of today’s infertility research revolves assisted reproductive technologies (ARTs) and methods to improve pregnancy success rates.
A recent development in this field is the time-lapse embryo imaging. With this technique, the developing embryos are kept constantly in an incubator and under a microscope that takes pictures every 10-20 minutes. The method can be used to select the healthiest-looking embryos, at the lowest risk of having chromosomal abnormalities based on their development, and to introduce those selected ones into the uterus for implantation (on the fifth day, as blastocysts). Time-lapse imaging, in fact a method for selective embryo transfer, can boost the success rate of IVF, according to British research.
Video about normal fertilization and conception (02:00)

Video about in-vitro fertilization (00:59)

Video about intra-uterine insemination (00:29)

Sources and Acknowledgements
- Eunice Kennedy Shriver National Institute of Child Health and Human Development at National Institutes of Health

