

Title of notification
A personalized refresher about kidney stones
What is a kidney stone?
A kidney stone is a solid piece of material that forms in a kidney when substances that are normally found in the urine become highly concentrated. A stone may stay in the kidney or travel down the urinary tract. Kidney stones vary in size. A small stone may pass on its own, causing little or no pain. A larger stone may get stuck along the urinary tract and can block the flow of urine, causing severe pain or bleeding.
Kidney stones are one of the most common disorders of the urinary tract. Each year in the United States, people make more than a million visits to health care providers and more than 300,000 people go to emergency rooms for kidney stone problems.
Urolithiasis is the medical term used to describe stones occurring in the urinary tract. Other frequently used terms are urinary tract stone disease and nephrolithiasis. Terms that describe the location of the stone in the urinary tract are sometimes used. For example, a ureteral stone—or ureterolithiasis—is a kidney stone found in the ureter.
What is the urinary tract?

Who gets kidney stones?
Anyone can get a kidney stone, but some people are more likely to get one. Men are affected more often than women, and kidney stones are more common in non-Hispanic white people than in non-Hispanic black people and Mexican Americans. Overweight and obese people are more likely to get a kidney stone than people of normal weight. In the United States, 8.8 percent of the population, or one in 11 people, have had a kidney stone.
What causes kidney stones?
Kidney stones can form when substances in the urine—such as calcium, oxalate, and phosphorus—become highly concentrated. The body uses food for energy and tissue repair. After the body uses what it needs, waste products in the bloodstream are carried to the kidneys and excreted as urine. Diet is one of several factors that can promote or inhibit kidney stone formation. Certain foods may promote stone formation in people who are susceptible, but scientists do not believe that eating any specific food causes stones to form in people who are not susceptible. Other factors that affect kidney stone formation include genes, environment, body weight, and fluid intake.
- hypercalciuria, a condition that runs in families in which urine contains unusually large amounts of calcium; this is the most common condition found in those who form calcium stones.
- a family history of kidney stones.
- cystic kidney diseases, which are disorders that cause fluid-filled sacs to form on the kidneys.
- hyperparathyroidism, a condition in which the parathyroid glands, which are four pea-sized glands located in the neck,release too much hormone, causing extra calcium in the blood.
- renal tubular acidosis, a disease that occurs when the kidneys fail to excrete acids into the urine, which causes a person' s blood to remain too acidic.
- cystinuria, a condition in which urine contains high levels of the amino acid cystine.
- hyperoxaluria, a condition in which urine contains unusually large amounts of oxalate.
- hyperuricosuria, a disorder of uric acid metabolism.
- gout, a disorder that causes painful swelling of the joints.
- blockage of the urinary tract.
- chronic inflammation of the bowel.
- a history of gastrointestinal (GI) tract surgery.
Others at increased risk of kidney stones are people taking certain medications including:
- diuretics-medications that help the kidneys remove fluid from the body
- calcium-based antacids
- the protease inhibitor indinavir (Crixivan), a medication used to treat HIV infection
- the anti-seizure medication topiramate (Topamax)
What are the types of kidney stones?
Four major types of kidney stones can form:
- Calcium stones are the most common type of kidney stone and occur in two major forms: calcium oxalate and calcium phosphate. Calcium oxalate stones are more common. Calcium oxalate stone formation may be caused by high calcium and high oxalate excretion. Calcium phosphate stones are caused by the combination of high urine calcium and alkaline urine, meaning the urine has a high pH.
- Uric acid stones form when the urine is persistently acidic. A diet rich in purines—substances found in animal protein such as meats, fish, and shellfish—may increase uric acid in urine. If uric acid becomes concentrated in the urine, it can settle and form a stone by itself or along with calcium.
- Struvite stones result from kidney infections. Eliminating infected stones from the urinary tract and staying infection-free can prevent more struvite stones.
- Cystine stones result from a genetic disorder that causes cystine to leak through the kidneys and into the urine, forming crystals that tend to accumulate into stones.
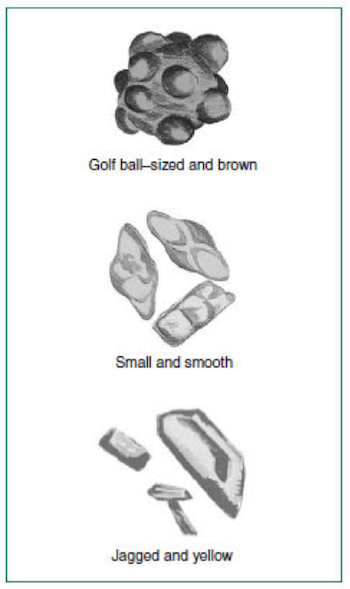
What do kidney stones look like?
Kidney stones vary in size and shape. Stones may be as small as a grain of sand or as large as a pearl. Some stones are even as big as golf balls. Stones may be smooth or jagged and are usually yellow or brown.
What are the symptoms of kidney stones?
People with kidney stones may have pain while urinating, see blood in the urine, or feel a sharp pain in the back or lower abdomen. The pain may last for a short or long time. People may experience nausea and vomiting with the pain. However, people who have small stones that pass easily through the urinary tract may not have symptoms at all.
How are kidney stones diagnosed?
To diagnose kidney stones, the health care provider will perform a physical exam and take a medical history. The medical history may include questions about family history of kidney stones, diet, GI problems, and other diseases and disorders. The health care provider may perform urine, blood, and imaging tests, such as an X-ray or computerized tomography (CT) scan to complete the diagnosis.
Urinalysis
Urinalysis is testing of a urine sample. The urine sample is collected in a special container in a health care provider’s office or commercial facility and can be tested in the same location or sent to a lab for analysis. Urinalysis can show whether the person has an infection or the urine contains substances that form stones.
Blood tests
A blood test involves drawing blood at a health care provider’s office or commercial facility and sending the sample to a lab for analysis. The blood test can show biochemical problems that can lead to kidney stones.
Abdominal X-rays
An abdominal X-ray is a picture created using radiation and recorded on film or on a computer. The amount of radiation used is small. An X-ray is performed at a hospital or outpatient center by an X-ray technician, and the images are interpreted by a radiologist—a doctor who specializes in medical imaging. Anesthesia is not needed. The person will lie on a table or stand during the X-ray. The X-ray machine is positioned over the abdominal area. The person will hold his or her breath as the picture is taken so that the picture will not be blurry. The person may be asked to change position for additional pictures. The X-rays can show the location of stones in the kidney or urinary tract.
CT scan
CT scans use a combination of X rays and computer technology to create three-dimensional (3-D) images. A CT scan may include the injection of a special dye, called contrast medium. CT scans require the person to lie on a table that slides into a tunnel-shaped device where the X rays are taken. The procedure is performed in an outpatient center or hospital by an X-ray technician, and the images are interpreted by a radiologist. Anesthesia is not needed. CT scans can show stone locations and conditions that may have caused the stone to form.
How are kidney stones treated?


Treatment for kidney stones usually depends on their size and what they are made of, as well as whether they are causing pain or obstructing the urinary tract. Kidney stones may be treated by a general practitioner or by a urologist—a doctor who specializes in the urinary tract. Small stones usually pass through the urinary tract without treatment. Still, the person may need pain medication and should drink lots of fluids to help move the stone along. Pain control may consist of oral or intravenous (IV) medication, depending on the duration and severity of the pain. IV fluids may be needed if the person becomes dehydrated from vomiting or an inability to drink. A person with a larger stone, or one that blocks urine flow and causes great pain, may need more urgent treatment, such as shock wave lithotripsy, uteteroscopy, or percutaneous nephrolithotomy.
Shock wave lithotripsy
A machine called a lithotripter is used to crush the kidney stone. The procedure is performed by a urologist on an outpatient basis and anesthesia is used. In shock wave lithotripsy, the person lies on a table or, less commonly, in a tub of water above the lithotripter. The lithotripter generates shock waves that pass through the person’s body to break the kidney stone into smaller pieces to pass more readily through the urinary tract.
Ureteroscopy
A ureteroscope—a long, tube-like instrument with an eyepiece—is used to find and retrieve the stone with a small basket or to break the stone up with laser energy. The procedure is performed by a urologist in a hospital with anesthesia. The urologist inserts the ureteroscope into the person’s urethra and slides the scope through the bladder and into the ureter. The urologist removes the stone or, if the stone is large, uses a flexible fiber attached to a laser generator to break the stone into smaller pieces that can pass out of the body in the urine. The person usually goes home the same day.
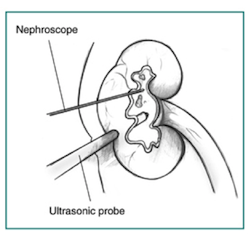
Percutaneous nephrolithotomy
In this procedure, a wire-thin viewing instrument called a nephroscope is used to locate and remove the stone. The procedure is performed by a urologist in a hospital with anesthesia. During the procedure, a tube is inserted directly into the kidney through a small incision in the person’s back. For large stones, an ultrasonic probe that acts as a lithotripter may be needed to deliver shock waves that break the stone into small pieces that can be removed more easily. The person may have to stay in the hospital for several days after the procedure and may have a small tube called a nephrostomy tube inserted through the skin into the kidney. The nephrostomy tube drains urine and any residual stone fragments from the kidney into a urine collection bag. The tube is usually left in the kidney for 2 or 3 days while the person remains in the hospital.
How are kidney stones prevented?
Why is knowing which type of kidney stone a person has important?
The first step in preventing kidney stones is to understand what is causing the stones to form. This information helps the health care provider suggest diet changes to prevent future kidney stones. For example, limiting oxalate in the diet may help prevent calcium oxalate stones but will do nothing to prevent uric acid stones. Some dietary recommendations may apply to more than one type of stone. Most notably, drinking enough fluids helps prevent all kinds of kidney stones by keeping urine diluted and flushing away materials that might form stones.
How does a health care provider determine the type of kidney stone?
If a person can catch a kidney stone as it passes, it can be sent to a lab for analysis. Stones that are causing symptoms can be retrieved surgically or with a scope inserted through the urethra into the bladder or ureter, then sent to a lab for analysis.
Blood and urine can also be tested for unusual levels of chemicals such as calcium, oxalate, and sodium to help determine what type of kidney stone a person may have had. The health care provider may ask the person to collect urine for 24 hours after a stone has passed or been removed to measure daily urine volume and mineral levels. Producing too little urine or having a mineral abnormality can make a person more likely to form stones.
Kidney stones may be prevented through changes in eating, diet, and nutrition and medications.
Eating, Diet, and Nutrition
People can help prevent kidney stones by making changes in their fluid intake. Depending on the type of kidney stone a person has, changes in the amounts of sodium, animal protein, calcium, and oxalate consumed can also help.
Drinking enough fluids each day is the best way to help prevent most types of kidney stones. Health care providers recommend that a person drink 2 to 3 liters (2 or 3 quarts) of fluid a day. People with cystine stones may need to drink even more. Though water is best, other fluids may also help prevent kidney stones, such as citrus drinks.

Recommendations specific to calcium oxalate stones include the following:
- reducing sodium
- reducing animal protein, such as meat, eggs, and fish
- getting enough calcium from food or taking calcium supplements with food
- avoiding foods high in oxalate, such as spinach, rhubarb, nuts, and wheat bran
Recommendations specific to calcium phosphate stones include the following:
- reducing sodium
- reducing animal protein
- getting enough calcium from food or taking calcium supplements with food
Recommendations specific to uric acid stones include limiting animal protein.
How much fluid should a person drink to prevent kidney stone formation?
People who have had a kidney stone should drink enough water and other fluids to produce at least 2 liters (2 quarts) of urine a day. People who have had cystine stones may need to drink even more. The amount of fluid each person needs to drink depends on the weather and the person’s activity level—people who work or exercise in hot weather need more fluid to replace the fluid they lose through sweat. A 24-hour urine collection may be used to determine the volume of urine produced during a day. If the volume of urine produced is too low, the person can be advised to increase fluid intake. Drinking enough fluid is the most important thing a person can do to prevent kidney stones.
Some studies suggest citrus drinks like lemonade and orange juice protect against kidney stones because they contain citrate, which stops crystals from growing into stones.
How does sodium in the diet affect kidney stone formation?
Sodium, often from salt, causes the kidneys to excrete more calcium into the urine. High concentrations of calcium in the urine combine with oxalate and phosphorus to form stones. Reducing sodium intake is preferred to reducing calcium intake.
The U.S. recommended dietary allowance (RDA) of sodium is 2,300 milligrams (mg), but Americans’ intake averages 3,400 mg, according to the U.S. Department of Agriculture. The risk of kidney stones increases with increased daily sodium consumption. People who form calcium oxalate or calcium phosphate stones should limit their intake to the U.S. RDA level, even if they take medications to prevent kidney stones.
How can a person limit sodium intake?
Learning the sodium content of foods can help people control their sodium intake. Food labels provide information about sodium and other nutrients. Keeping a sodium diary can help a person limit sodium intake to 2,300 mg. When eating out, people should ask about the sodium content of the foods they order.
Some foods have such large amounts of sodium that a single serving provides a major portion of the RDA. Foods that contain high levels of sodium include:
- hot dogs
- canned soups and vegetables
- processed frozen foods
- luncheon meats
- fast food
People who are trying to limit their sodium intake should check labels for ingredients and hidden sodium, such as:
- monosodium glutamate, or MSG
- sodium bicarbonate, the chemical name for baking soda
- baking powder, which contains sodium bicarbonate and other chemicals
- disodium phosphate
- sodium alginate
- sodium nitrate or nitrite,
How does animal protein in the diet affect kidney stone formation?
Meats and other animal protein—such as eggs and fish—contain purines, which break down into uric acid in the urine. Foods especially rich in purines include organ meats, such as liver. People who form uric acid stones should limit their meat consumption to 6 ounces (170 grams) each day.
Animal protein may also raise the risk of calcium stones by increasing the excretion of calcium and reducing the excretion of citrate into the urine. Citrate prevents kidney stones, but the acid in animal protein reduces the citrate in urine.
How does calcium in the diet affect kidney stone formation?
Calcium from food does not increase the risk of calcium oxalate stones. Calcium in the digestive tract binds to oxalate from food and keeps it from entering the blood, and then the urinary tract, where it can form stones. People who form calcium oxalate stones should include 800 mg of calcium in their diet every day, not only for kidney stone prevention but also to maintain bone density. A cup of low-fat milk contains 300 mg of calcium. Other dairy products such as yogurt are also high in calcium. For people who have lactose intolerance and must avoid dairy products, orange juice fortified with calcium or dairy with reduced lactose content may be alternatives. Calcium supplements may increase the risk of calcium oxalate stones if they are not taken with food.
How does oxalate in the diet affect kidney stone formation?
Some of the oxalate in urine is made by the body. However, eating certain foods with high levels of oxalate can increase the amount of oxalate in the urine, where it combines with calcium to form calcium oxalate stones. Foods that have been shown to increase the amount of oxalate in urine include spinach, rhubarb, nuts, and wheat bran. Avoiding these foods may help reduce the amount of oxalate in the urine.
What diet plan should a person follow to prevent future kidney stones?
A dietitian can help a person plan meals that lower the risk of forming stones based on the type of stone the person formed in the past. A person with a history of kidney stones may want to talk to a dietitian who specializes in kidney stone prevention or nutrition for people with kidney problems.
A dietitian can also help overweight people plan meals to help them lose weight. Studies have shown that being overweight increases the risk of kidney stones, particularly uric acid stones. Diets that are low in carbohydrates have been shown to further increase the risk of uric acid stones and should be avoided.
Studies have shown the Dietary Approaches to Stop Hypertension (DASH) diet can reduce the risk of kidney stones. The DASH diet is high in fruits and vegetables, moderate in low-fat dairy products, and low in animal protein. DASH is a flexible and balanced eating plan that helps creates a heart-healthy eating style for life. The DASH eating plan requires no special foods and instead provides daily and weekly nutritional goals. This plan recommends:
- Eating vegetables, fruits, and whole grains
- Including fat-free or low-fat dairy products, fish, poultry, beans, nuts, and vegetable oils
- Limiting foods that are high in saturated fat, such as fatty meats, full-fat dairy products, and tropical oils such as coconut, palm kernel, and palm oils
- Limiting sugar-sweetened beverages and sweets.
-
Based on these recommendations, the following table shows examples of daily and weekly servings that meet DASH eating plan targets for a 2,000-calorie-a-day diet:

When following the DASH eating plan, it is important to choose foods that are:
- Low in saturated and trans fats
- Rich in potassium, calcium, magnesium, fiber, and protein
- Lower in sodium
Medications
The health care provider may prescribe certain medications to help prevent kidney stones based on the type of stone formed or conditions that make a person more prone to form stones:
- hyperuricosuria—allopurinol (Zyloprim), which decreases uric acid in the blood and urine.
- hypercalciuria—diuretics, such as hydrochlorothiazide.
- hyperoxaluria—potassium citrate to raise the citrate and pH of urine.
- uric acid stones—allopurinol and potassium citrate.
- cystine stones—mercaptopropionyl glycine, which decreases cystine in the urine, and potassium citrate.
- struvite stones—antibiotics, which are bacteria-fighting medications, when needed to treat infections, or acetohydroxamic acid with long-term antibiotic medications to prevent infection.
People with hyperparathyroidism sometimes develop calcium stones. Treatment in these cases is usually surgery to remove the parathyroid glands. In most cases, only one of the glands is enlarged. Removing the glands cures hyperparathyroidism and prevents kidney stones.
Points to remember
- A kidney stone is a solid piece of material that forms in a kidney when substances that are normally found in the urine become highly concentrated.
- Kidney stones are one of the most common disorders of the urinary tract.
- Kidney stones can form when substances in the urine—such as calcium, oxalate, and phosphorus— become highly concentrated. Diet is one of several factors that can promote or inhibit kidney stone formation.
- Four major types of kidney stones can form: calcium stones, uric acid stones, struvite stones, and cystine stones.
- Certain foods may promote stone formation in people who are susceptible, but scientists do not believe that eating any specific food causes stones to form in people who are not susceptible.
- Drinking enough fluid is the most important thing a person can do to prevent kidney stones.
- People who have had a kidney stone should drink enough water and other fluids to make at least 2 liters of urine a day.
- Sodium, often from salt, causes the kidneys to excrete more calcium into the urine. High concentrations of calcium in the urine combine with oxalate and phosphorus to form stones. Reducing sodium intake is preferred to reducing calcium intake.
- Meats and other animal protein—such as eggs and fish—contain purines, which break down into uric acid in the urine.
- Calcium from food does not increase the risk of calcium oxalate stones. Calcium in the digestive tract binds to oxalate from food and keeps it from entering the blood, and then the urinary tract, where it can form stones.
- A dietitian can help a person plan meals that lower the risk of forming stones based on the type of stone the person formed in the past.
- People with kidney stones may have pain while urinating, see blood in the urine, or feel a sharp pain in the back or lower abdomen. However, people who have small stones that pass easily through the urinary tract may not have symptoms at all.
- To diagnose kidney stones, the health care provider will perform a physical exam and take a medical history. The health care provider may perform urine, blood, and imaging tests to complete the diagnosis.
- Treatment for kidney stones usually depends on their size and what they are made of, as well as whether they are causing pain or obstructing the urinary tract. Treatments may include Shock wave lithotripsy, Ureteroscopy, or Percutaneous nephrolithotomy.
- Kidney stones may be prevented through changes in eating, diet, and nutrition and medications.
Kidney stone research
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) funds research on the causes, treatments, and prevention of kidney stones. The International Registry for Hereditary Kidney Stone Diseases, funded under National Institutes of Health (NIH) clinical trial number NCT00588562, collects medical information from a large number of patients with kidney stones to create a registry that will help researchers compare similarities and differences in patients and their symptoms.
The Study of the Biological and Physical Manifestations of Spontaneous Uric Acid Kidney Stone Disease, funded under NIH clinical trial number NCT00904046, aims to determine how much fat accumulates within cells and how it affects the kidneys by correlating kidney fat content with urine test results. A second aim is to evaluate the effect of the medication thiazolidinedione on excess fatty acid accumulation in kidney tissue and its correlation with uric acid stone formation.
Tamsulosin for Urolithiasis in the Emergency Department, funded under NIH clinical trial number NCT00382265, studies the effectiveness and safety of tamsulosin in treatment of kidney stones. Other areas of focus include reduction in time to pain-free recovery, decrease in narcotic medication for pain, less need for follow-up, decrease in the need for surgery, and cost savings.
Clinical trials are research studies involving people. Clinical trials look at safe and effective new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses.
Sources and Acknowledgments
National Institutes of Health, U.S. Department of Health and Human Services. NIH Publication No. 13–2495, “Kidney Stones in Adults,” February 2013.
National Institutes of Health, U.S. Department of Health and Human Services. NIH Publication No. 13-6425, “Diet for Kidney Stone Prevention,” February 2013.
National Institutes of Health, U.S. Department of Health and Human Services. NIH Publication No. 13-4154, “What I Need to Know About Kidney Stones,” February 2013.
National Institutes of Health, U.S. Department of Health and Human Services. “Description of the DASH Eating Plan,” September 2015.
