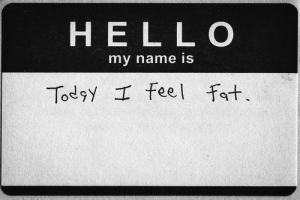
Do you like what you see in the mirror? Do you think “I am too fat?” or worry that “I can’t fit into my skinny jeans?”
 Many people do not have a positive body image. Research has focused on mass media images of the “perfect” thin body as part of the problem.
Many people do not have a positive body image. Research has focused on mass media images of the “perfect” thin body as part of the problem.
In a longitudinal experiment, college women were exposed to fashion magazines over a 15 month period. What happened? Those women who lacked social support, who started the experiment feeling dissatisfied with their body and who felt pressure to be thin were more likely to experience increased negative feelings about their body, increased dieting and eating disorder symptoms after long-term exposure to the magazines.
Another recent study found that exposure to Facebook could negatively impact ideas about body image in 13 to 15 year old girls.
Body Image and Eating Disorders
Puberty is identified as a critical period in the development of eating disorders because of the large changes in body shape that occur. For girls, the physical change includes increases in the amount of body fat and a widening of hips. During their teen years, girls and boys gain half of their adult body weight. Research indicates that peer pressure through weight related teasing and comparisons with peers are contributing factors in body dissatisfaction. Parental worries  about weight can also influence negative feelings about their weight in teenagers.
about weight can also influence negative feelings about their weight in teenagers.
Another factor that can influence the development of eating disorders has to do with thinking patterns. People who believe that goals like happiness or wellness cannot be achieved without first reaching lower order goals, like weight loss, are more likely to develop eating disorders.
Risky Behavior with Insulin
Although most adolescents do not develop eating disorders, some are at risk. For adolescents with Type 1 diabetes, body image can even become a critical factor in diabetes self-care. In fact, according to a 2015 journal article, as many as 40% of young adult women who have type 1 diabetes are intentionally reducing their the amount of insulin they take in order to prevent weight gain or to lose weight. Another review of the literature found that approximately one-third of people with type 1 diabetes intentionally omit insulin for weight control.
What is the mechanism that causes this weight loss?
How Insulin Works
When you eat food, the pancreas detects the presence of glucose, fatty acids and amino acids in the small intestines. It secretes insulin into the bloodstream. Insulin tells the cells of the body to absorb glucose and other nutrients from the blood. Insulin also acts on the liver, telling it to start building glycogen (a way the body stores glucose) from glucose in the blood. Thus insulin, in effect, lowers the amount of sugar in your blood.
 Being insulin dependent means that you need to inject insulin in your body. This is because either the islets of Langerhans in the pancreas have been destroyed by your immune system as in Type 1 Diabetes or your body’s cells do not respond to the insulin your pancreas produces as in Type 2 Diabetes and you need to inject insulin.
Being insulin dependent means that you need to inject insulin in your body. This is because either the islets of Langerhans in the pancreas have been destroyed by your immune system as in Type 1 Diabetes or your body’s cells do not respond to the insulin your pancreas produces as in Type 2 Diabetes and you need to inject insulin.
Without insulin your cells cannot absorb glucose. Glucose leaves the body as waste flowing into the urine.
Many people are first diagnosed with type one diabetes because they have symptoms of fatigue, excessive weight loss and increased urination. In this case, people who restrict their insulin are instigating these same symptoms.
Type One Diabetes Without Insulin
Without insulin, glucose cannot get into the cells. High blood glucose results. But additionally the body goes into “starvation” mode: cells begin to burn fat. Ketones are produced. In time, the tissues of the body and the blood stream become acidic. This is called ketoacidosis.
Skipping insulin for weight loss is dangerous. The short-term results are dehydration, fatigue and loss of muscle tissue. The long term implications are kidney damage, blindness and heart disease, coma and death.
Difficult to Diagnose
Since food and measuring must be a focus of living with type one diabetes, it shouldn’t be surprising that eating disorders occur. Eating disorders are notoriously hard to diagnose and treat. In this case, insulin restriction behaviors are even harder to identify because they look like poor diabetes control.
Determining the amount and timing of insulin—especially when adding in the complications of your activity level, amounts of food you eat, amount of stress you are experiencing, illness and more—can seem impossible. Many people feel that they are just one step behind their diabetes, always correcting for highs (high blood glucose levels) and/or lows (low blood glucose levels).
Long-term Impact of Insulin Restriction Behaviors
 A study with results published in 2007 and in 2011 tells a bleak story of the long-term results of insulin restrictions for weight loss. The researchers surveyed at two different times, baseline and 11 years later. Women with Type 1 diabetes who practiced insulin restriction were three times more likely to have died over the course of the 11 years than those who took their insulin appropriately. In addition, their lives were shortened by 13 years compared to their counterparts who took their insulin appropriately.
A study with results published in 2007 and in 2011 tells a bleak story of the long-term results of insulin restrictions for weight loss. The researchers surveyed at two different times, baseline and 11 years later. Women with Type 1 diabetes who practiced insulin restriction were three times more likely to have died over the course of the 11 years than those who took their insulin appropriately. In addition, their lives were shortened by 13 years compared to their counterparts who took their insulin appropriately.
Those with this eating disorder were also more likely to have complications like kidney damage and foot problems than their counterparts. Fear of weight gain when taking insulin appropriately and problems with diabetes self-care were instrumental in the women continuing to restrict their insulin.
Risk Factors or Signs of Developing Insulin Restriction Behaviors
People with eating disorders tend to conceal or deny their behaviors. This particular disorder is easy to hide because it is can be masked as poor diabetic management. A review of the literature identified eight signs or risk factors for the development of insulin restriction eating disorder in Type one diabetes.
Weight gain when starting insulin treatment
Overly restrictive dietary restraints, depriving approaches to eating, leading to binging and craving of forbidden foods.
![]()
Hypoglycemic episodes that happen on a regular basis. These repeated events are caused by the difficult balancing act of diabetes management around exercise, stress, insulin and food.
Depression or depressive feelings are twice as likely among people with type 1 diabetes as the general population.
![]()
Frequently high HbA1c levels and diabetic ketosis
Preoccupation with appearance
Frequently missed doctor’s appointments
![]()
Refusal to be weighed at the doctor’s office
Being alert to the signs of this eating disorder and getting treatment early can reduce complications and possible death from misuse of insulin.








I have a different problem…I see myself as not completely thin,but with a normal body. I should have more mirrors around so that I can see my whole body. My face does not bother me, because it does not look fat. While everything else does. I am not on insulin, but have been. Not for long, just to help get my sugars down at times. This is a weird situation for me? I have lost some weight (75lbs) in 2010 dealing with uterine cancer and I am free of cancer as of this day. I want to lose another 100 lbs…in time. I keep staying at the same weight. I would like to quit most of these pills I take. They are helping me keep my sugar down. I try not to cheat but I do at times. Sweets ! Ate them since very young. Can you all help with these things? My right foot/ankle I have Charcot foot deformity from driving a school bus for 13 yrs and had to take on another job sitting. My arthritis is very bad and my lower back works with me most times. I keep my wheel chair nearby if constant standing is needed. On and on…… I have a lot of little things going on. My heart is another. Not bad, just pills. Can you write to me on these things?
I have T1D x 48 yrs. I have an eating disorder. How do I get help?!
Hi Tina, There is a National Eating Disorders Hotline and Treatment Referral list at http://www.nationaleatingdisorders.org/ Recognizing the problem is a first step. Be sure to communicate with your physician. Best, Kathleen
This is a wonderfully written tutorial on Diabetes and the issues of insulin and diabetes management. Extremely helpful. Thank you!